Pavlidis ET, Pavlidis TE. Pathophysiological consequences of obstructive jaundice and perioperative management. Hepatobiliary Pancreat Dis Int. 2018 Feb;17(1):17-21.
Full-text for Emory users.
“Proper management includes full replacement of water and electrolyte deficiency, prophylactic antibiotics, lactulose, vitamin K and fresh frozen plasma, albumin and dopamine. The preoperative biliary drainage has not been indicated in overall, but only in a few selected cases.”
“The coagulation disorders and the resulting hemostasis impairment have been attributed to the complement activation by endotoxin as well as to the reduced synthesis of prothrombin (factor II) in the liver and the other vitamin K depended coagulation factors i.e. VII, IX, X and proteins C, S, Z. The absence of bile salts in the gut prevents the absorption of vitamin K, which is a fat-soluble vitamin. In addition, the endogenous microbial flora produces small amounts of vitamin K. Subsequently the reduced vitamin K absorption results in its deficiency. The latter predisposes to bleeding diathesis, despite the normal laboratory indices such as prothrombin time (PTT) and international normalized ratio (INR). Likewise, the other fat-soluble vitamin D and lipids absorption is diminished resulting in their deficiency and calcium reduction.” (Pavlidis, et al., p. 19.)
Cakir T, Cingi A, Yeğen C. Coagulation dynamics and platelet functions in obstructive jaundiced patients. J Gastroenterol Hepatol. 2009 May;24(5):748-51.
Full-text for Emory users.
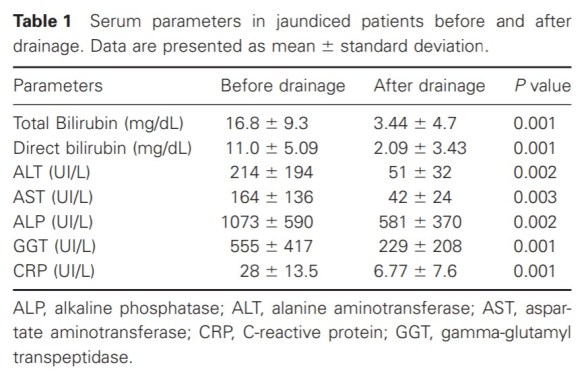
Results: Hypercoagulation was detected in 80% of patients. Maximum strength, elasticity, coagulation indices of the clot were correlated with increased concentrations of direct bilirubin. Although maximum strength of coagulum usually represents increased activity of platelet function, membrane closure times with PFA 100 were found to be prolonged in 30% of patients, reduced values were determined in 17% of patients. No demonstrable effect on coagulation parameters and platelet function were detected after drainage procedures regardless of modality.
Conclusions: Even though there is a general assumption about the increased bleeding tendency in obstructive jaundiced patients, we could not demonstrate reduced clotting activity by measuring with either PFA or TEG. On the contrary we observed tendency for hypercoagulation independent of increased prothrombin times. The most probable cause of this effect is the increased activity of fibrin polymers on platelet membrane.
Papadopoulos V, Filippou D, Manolis E, Mimidis K. Haemostasis impairment in patients with obstructive jaundice. J Gastrointestin Liver Dis. 2007 Jun;16(2):177-86.
Abstract: As part of the multifactorial role of liver in protein synthesis, many coagulation factors, natural anticoagulants, and compounds of the fibrinolytic system are produced in the liver. A prolonged liver disease, either biliary obstruction or parenchymal liver disease, is consecutively accompanied by abnormal clotting. In the present paper we review the haemostasis impairment in obstructive jaundice with special reference to the hepatic cirrhosis and failure, to systemic inflammation and sepsis that develops in cholestatic diseases, and finally in some other benign or malignant diseases including pancreatic adenocarcinoma, acute pancreatitis, cholangiocarcinoma, and hepatocellular carcinoma. Finally, a special reference to the possible therapeutic interventions has been made. […] Understanding the pathophysiology of haemostatic changes in patients with cholestasis, and, more generally, liver disease, is the hallmark of accurate diagnosis and treatment.
More PubMed results on obstructive jaundice and coagulation disorders.