“Palliative care (PC) interventions in the critically ill have been associated with reduced subsequent ICU admissions and reduced ICU length of stay. Barriers to PC integration
and utilization in the ICU include unrealistic expectations of ICU interventions by patients and families, barriers related to ICU culture as well as cultural attributes of patients and families, insufficient training in PC principles for ICU clinicians, PC workforce shortages,
and inability of patients to participate in treatment discussions. Overcoming these barriers and assessing patient and provider needs for specialty PC depends on the availability and capabilities of PC services at the institutional level, the bandwidth of providers and characteristics of the patient population.”
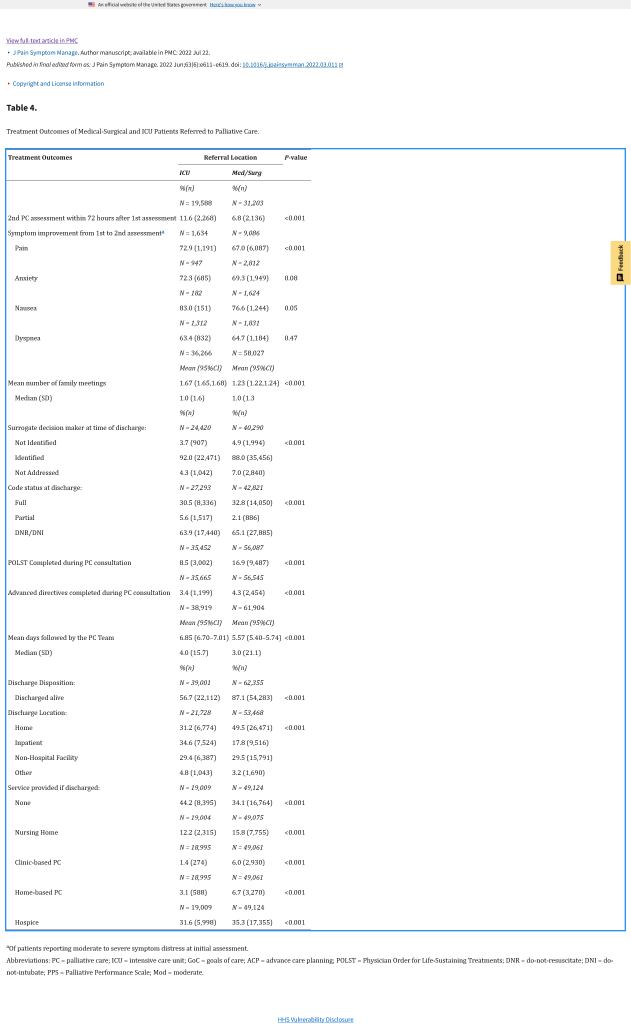
“This study highlights that patients receiving PC consultation in the ICU are sicker, more
likely to die, and less likely to be able to communicate than those on medical surgical units. The majority of PC consults in the ICU are for GOC and ACP support though specialty PC teams also improve pain and dyspnea. PC teams provide longitudinal care and address
a broad range of PC needs for ICU patients. Routine involvement of PC for patients with serious life-limiting conditions on admission to the ICU could allow more patients to participate in GOC conversations, earlier implementation of care decisions, and more effective management of symptoms.”
Chapman, Allyson Cook et al. “Utilization and Delivery of Specialty Palliative Care in the ICU: Insights from the Palliative Care Quality Network.” Journal of pain and symptom management vol. 63,6 (2022): e611-e619. Free Full Text
