Ulcerative colitis is characterized by mucosal ulceration, rectal bleeding, diarrhea, and abdominal pain. Pharmacologic management of ulcerative colitis has relied mainly on 5-aminosalicylates, corticosteroids, and immunosuppressants, including purine antimetabolites and cyclosporine. Corticosteroid dependence is a clinically important problem; furthermore, the probability of colectomy within the first five years after diagnosis ranges from 9 percent in patients with distal colitis to 35 percent in patients with total colitis, most commonly because of failed medical therapy. The cumulative risk of recurrent inflammatory bowel disease in the form of pouchitis ranges from 15.5 percent one year after the procedure to 45.5 percent 10 years after the procedure. Accordingly, new treatments for ulcerative colitis are needed.”
“Inducing and maintaining a clinical response and clinical remission and minimizing the use of corticosteroids are unmet goals in the treatment of patients with ulcerative colitis, particularly those who have not had a response to corticosteroids, azathioprine, or mercaptopurine. Our results show that infliximab is effective in patients who have mod-
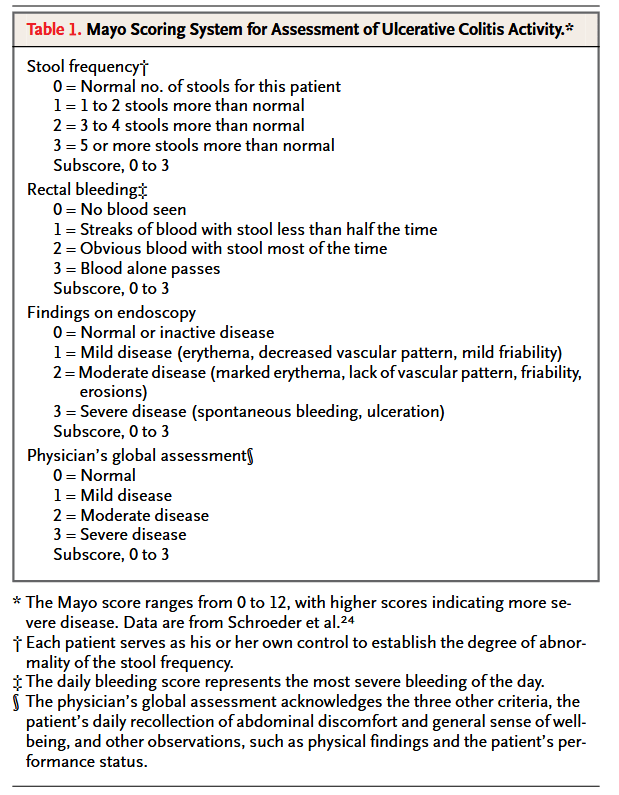
erate-to-severe disease despite the use of conventional therapy, in terms of a clinical response and remission. As compared with patients who received placebo, patients who received infliximab were significantly more likely to have a clinical response and be in clinical remission at weeks 8 and 30 in both trials and in week 54 in ACT 1. Similarly, patients who received infliximab were significantly more likely to have mucosal healing at weeks 8 and 30 in both trials and in week 54 in ACT 1. These findings are of particular importance in light of the recent suggestion that mucosal healing is the strongest predictor of a reduced risk of cancer among patients with ulcerative colitis.”
Rutgeerts, Paul et al. “Infliximab for induction and maintenance therapy for ulcerative colitis.” The New England journal of medicine vol. 353,23 (2005): 2462-76. Full Text for Emory Users
