“Medication discrepancies and errors occurring during hospital discharge represent a critical
concern, posing significant risks such as adverse patient outcomes, medication-related
readmissions, and increased health care costs. Pharmacist-led medication reconciliation
at discharge (PMRD) has emerged as a potential solution to enhance medication safety by
mitigating medication errors and reducing hospital readmissions.
Hospital discharge is a phase of care in which patients often become more vulnerable
due to the absence of monitoring and assistance with medication administration. Previous
publications from the Multi-Center Medication Reconciliation Quality Improvement Study
(MARQUIS) have revealed a reduction in potentially harmful discrepancies in admission
and discharge orders through a multifaceted medication reconciliation implementation
model.8,9 However, these studies did not further assess the unintentional discrepancies that
were identified, leaving a gap in understanding their potential for patient harm. While
Muller and colleagues have evaluated potential patient harm avoided through pharmacist
intervention in resolving discharge medication reconciliation discrepancies, there remains a
need for further investigation into the financial implications of such interventions.”
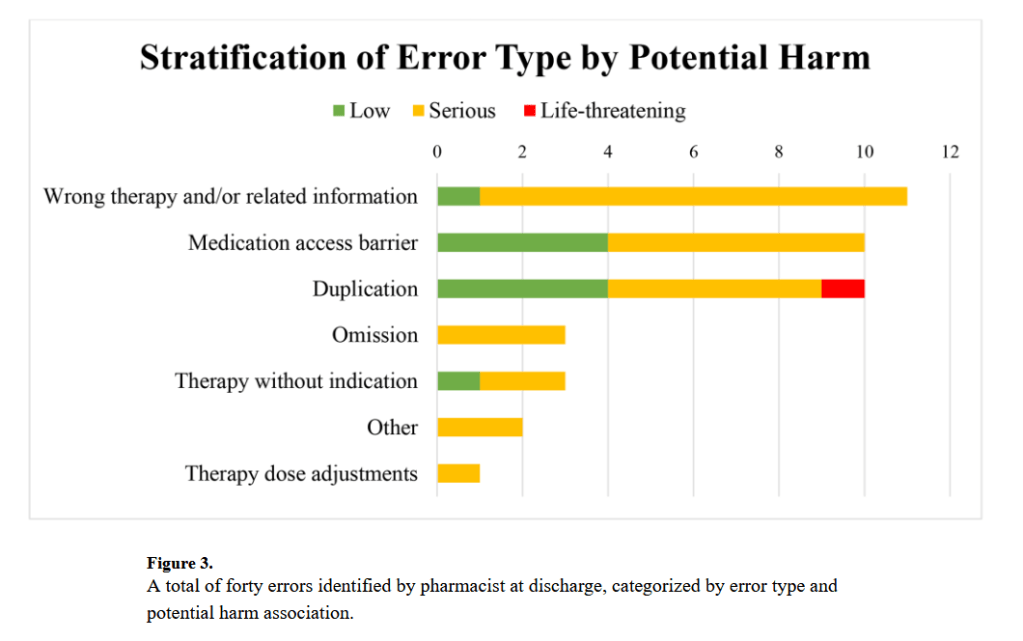
“Given that medication errors are prevalent during this discharge process, characterizing
the quantity and type of error, as well as the associated harm prevented, is crucial in
understanding the impact of a standard PMRD process on patient safety. In our study, we
utilized a simplified approach by applying an adapted NCC MERP Medication Error Index
to describe potential harm and coupled that with physician consultation on the likelihood
of an emergency department visit or hospital readmission. This was similar to Hoffman and
colleagues’ study, which also utilized an adapted NCC MERP Medication Error Index to
describe the potential harm that would reach patients; however, their primary end point
focused on cost avoidance, which they calculated via a sophisticated risk assignment
rubric.14 While this risk rubric tool allowed for important identification of the errors with
the greatest potential risk and cost avoidance, the actual pharmacist intervention rate was
much lower than what our study demonstrated (36% vs 68%). This difference may be due
to the integrated pharmacist model our study utilized in our PMRD process that capitalized
on interprofessional collaboration. Pharmacists in this study were involved throughout the
entirety of a patient’s hospital stay. By actively engaging in all stages of the patient’s
hospital journey, these pharmacists contributed to the delivery of high-quality, patient-
centered care and promoted optimal medication safety and management. However, this
workflow may be resource-intensive and limited by institution-specific workload distribution
and resource allocation.”
Zheng, Linda et al. “Impact of pharmacist-led discharge medication reconciliation on error and patient harm prevention at a large academic medical center.” Journal of the American College of Clinical Pharmacy : JACCP vol. 7,8 (2024): 787-794. Free Full Text
