“There is evidence of endothelial dysfunction and a dysregulation of coagulation and fibrinolysis in individuals with HIV. In a study of 109 HIV-infected patients with advanced disease, 10% developed venous thrombosis and 6% developed arterial thrombosis. A variety of laboratory abnormalities were reported, including protein C deficiency, increased factor VIII concentrations, high fibrinogen concentrations, and free protein S deficiency. HIV infection is also associated with an increased D-dimer level, which suggests that HIV infection might be associated with a pro-thrombotic state. HIV disease is theorized to produce a pro-thrombotic state through mechanisms related to activation of the innate and adaptive immune system by low level HIV replication, co-pathogens, and microbial products trans-located from the gastrointestinal tract,”
“The impact of HAART on coagulation is unclear. Protease inhibitors (PI) have been associated with higher fibrinogen levels and lipodystrophy. PIs are also thought to interfere with cytochrome P (CYP) 450 metabolism and regulation of thrombotic proteins. This may
cause a pro-thrombotic state in HIV-infected individuals”
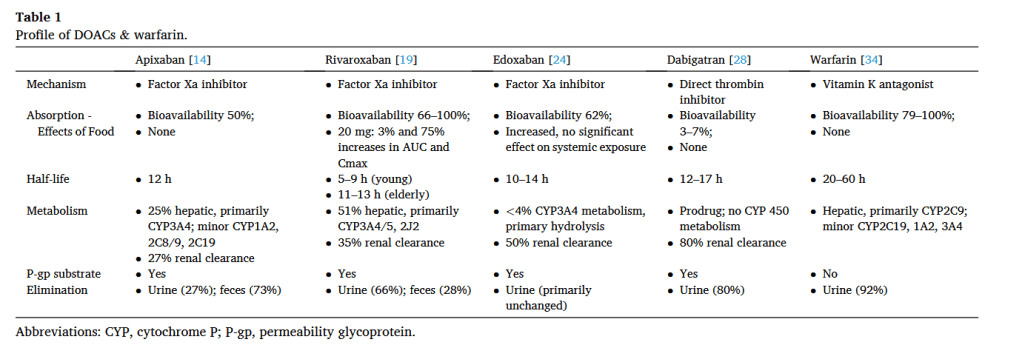
“This review may assist providers with therapy selection and monitoring. Since the aging population may have been diagnosed earlier and maintained on other agents that were previously first line, such as PIs or NNRTIs, DDI are possible and must be considered. Although data is limited, the potential for DDIs between HAART and DOACs exists based
on PK profiles. The commonly used DOACs are metabolized through CYP450 enzymes, and/or are substrates of P-gp transporters, or undergo renal excretion. Management of these interactions should involve careful clinical selection based on patient characteristics. When possible, HAART and DOACs with a low potential for DDI should be selected. In
the setting of DDI, warfarin remains a viable anticoagulant choice as one can monitor the INR (more closely, if required) to ensure a therapeutic INR is achieved for the indicated treatment. As new information continues to emerge, readers are advised to consult drug interaction resources.”
Sabourin AA, Patel T, Saad S, Renner E, Mouland E, Adie S, Ha NB. Management of anticoagulation in patients with human immunodeficiency virus/acquired immunodeficiency virus. Thromb Res. 2021 Apr;200:102-108. doi: 10.1016/j.thromres.2021.01.020. Epub 2021 Jan 27. Full Text for Emory Users
