“Thyrotoxicosis has been reported as a postoperative complication of parathyroidectomy
(PTx), attributed to palpation thyroiditis. Palpation thyroiditis was first described by Carney et al., in 1975 as a pathologic response to the traumatic injury of thyroid follicles, characterized by multifocal granulomatous folliculitis. The existing cohort studies in post-PTx thyrotoxicosis are limited. A prospective study of patients who underwent PTx for primary and secondary HPT reported that the incidence rate of thyrotoxicosis after PTx was 31.2 % and 77 %, respectively. The clinical significance of post-PTx thyrotoxicosis remains controversial. While
various manifestations of thyrotoxicosis, including tremors, palpitations, new-onset atrial fibrillation, and angina pectoris mimicking myocardial infarction, were described by case reports, Stang et al. in a cohort study reported that only 15 % of patients developed symptoms of thyrotoxicosis 1–2 weeks after the operation. They further concluded
that the degree of neck dissection appeared explanatory but did not specify which maneuvers were contributory.”
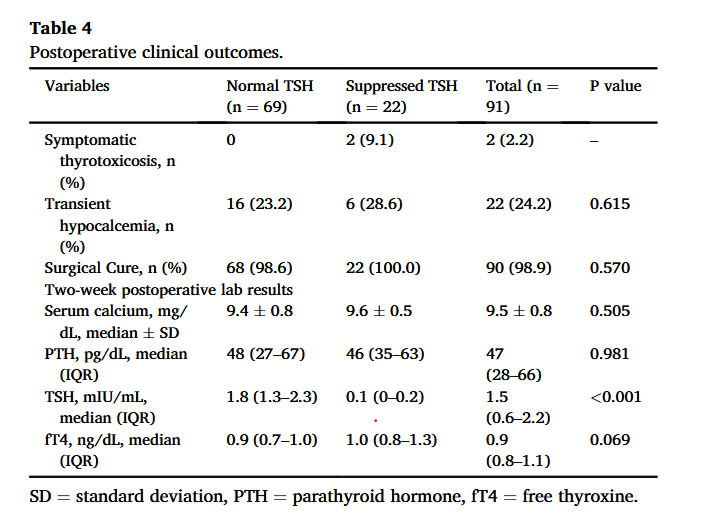
“Many case reports have described thyrotoxicosis after PTx. However, existing cohort studies are limited. The reported incidence rate of post-PTx thyrotoxicosis ranged widely from 31 % to 77 %, likely due to the difference in surgical technique, timing of postoperative follow-ups, and definition of thyrotoxicosis. Lindblom et al.prospectively reviewed 26 patients who underwent PTx for primary HPT and found that 42.3 % had an elevated T4 and triiodothyronine (T3) on the first and/or fourth postoperative day. Stang et al. reported that 31.2 % of patients who underwent PTx for primary HPT had a suppressed TSH 7–14vweeks after the operation. Rudofsky et al. reported a higher incidence rate of 77 % among patients undergoing PTx for secondary HPT. In their study, all patients underwent bilateral neck exploration and obtained thyroid function tests (TSH, fT3, and fT4) on postoperative days 1, 3, 5, 10, and 40.
Our study found that 24 % of patients developed thyrotoxicosis following PTx, which was mostly asymptomatic. If PTx is attributed to postoperative thyrotoxicosis, the lower incidence rate was likely due to our surgical techniques and the timing of postoperative follow-ups. We
intentionally minimized the manipulation of the thyroid gland and used a Kittner clamp for retraction. Patients in our study routinely obtained thyroid function tests 2 weeks after PTx, which was later than in other studies. The half-life of TSH and T4 is 55 min and 7 days, respectively. Patients with transient thyrotoxicosis that resolved within 2 weeks were
not captured in our study.”
Wang, Rongzhi et al. “Retracting the thyroid matters: Who develops asymptomatic transient thyrotoxicosis after parathyroidectomy.” American journal of surgery vol. 230 (2024): 9-13. Full Text for Emory Users
