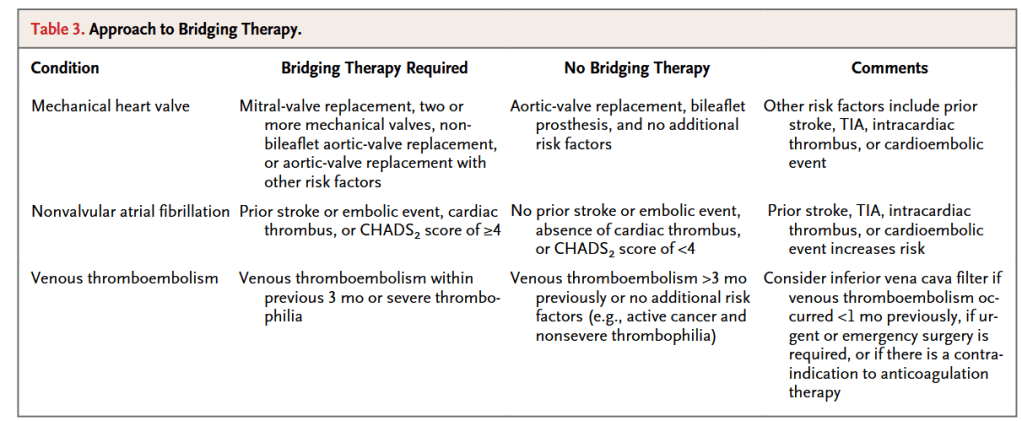
“The question of whether antithrombotic therapy should be suspended in a patient who
will be undergoing an invasive procedure involves balancing the risk of postproce-
dural bleeding with continued treatment against the thrombotic risk with suspension
of treatment and use of bridging anticoagulation therapy. In general, a patient under-
going a procedure that is associated with a low risk of bleeding (low-risk procedure)
can safely continue antithrombotic therapy and should do so, particularly if the pa-
tient is at high risk for a thromboembolic event (high-risk patient). Conversely, a pa-
tient undergoing a high-risk procedure can temporarily discontinue antithrombotic
agents safely if the patient is at low risk for a thromboembolic event (low-risk patient).”
“For patients receiving long-term antithrombotic therapy, the approach to periprocedural use of antithrombotic agents needs to be individualized. Patients should be involved in the decision making process, especially when definitive recommendations cannot be made.”
“Key steps for safe and successful periprocedural management of antithrombotic therapy
are outlined in the Supplementary Appendix. Communication among health care providers
and a generally conservative approach are paramount. Whenever possible, procedures should be postponed until the risks associated with discontinuing anticoagulation therapy are as low as possible. Overly aggressive and premature reinstitution of antithrombotic therapy may result in bleeding. This can paradoxically lead to an increase in thrombotic events because of the need to reverse the antithrombotic effects, administer blood products, and postpone the reinitiation of antithrombotic therapy.”
Baron, Todd H et al. “Management of antithrombotic therapy in patients undergoing invasive procedures.” The New England journal of medicine vol. 368,22 (2013): 2113-24. Full Text for Emory Users
