“Colorectal cancer is the second-leading cause of cancer-related mortality in both the United States and Europe. With respect to prognosis, increasing evidence has suggested that systemic inflammation is a key predictor of disease progression and survival for colorectal cancer patients undergoing surgery. Furthermore, whereas red blood cell (RBC) transfusions may be life-saving in some circumstances, there has been growing evidence that transfusions are associated with adverse postoperative outcomes, including infectious complications and cancer recurrence. These detrimental effects are thought to be related to systemic inflammation and transfusion-related immunomodulation (TRIM). Whereas the exact mechanisms remain unknown, TRIM seems to be related to various immunologic changes, including decreased interleukin (IL)-2 production, monocyte and cytotoxic cell activity inhibition, increased suppressor T-cell activity, and immunosuppressive prostaglandin release.”
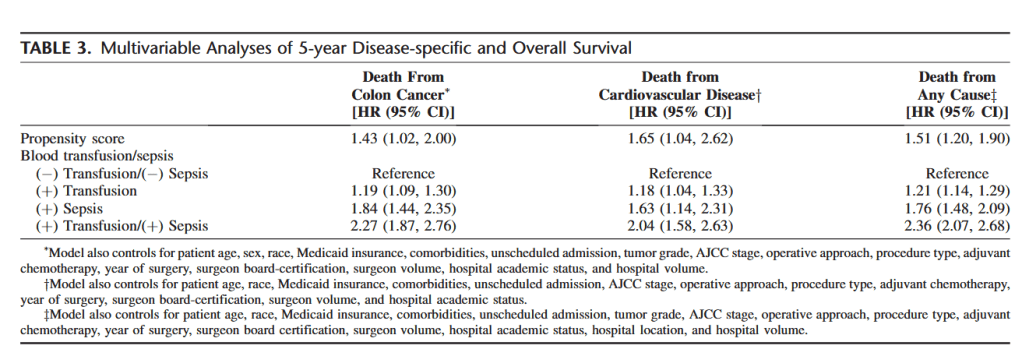
“This study found that preoperative and postoperative blood transfusions are independently associated with worse colon cancer DSS, cardiovascular DSS, and overall survival after potentially curative colon cancer resection. This finding was independent of sepsis, and an additive detrimental effect of both receipt of a transfusion and development of sepsis on survival was observed. However, no difference in colon cancer DSS or overall survival was
observed between those who received a preoperative transfusion and those who did not receive a transfusion. For cardiovascular DSS, the timing of the transfusion did not have an effect, because preoperative, intraoperative, and postoperative transfusions were each associated with worse survival.”
Aquina, Christopher T et al. “Association Among Blood Transfusion, Sepsis, and Decreased Long-term Survival After Colon Cancer Resection.” Annals of surgery vol. 266,2 (2017): 311-317. Full Text for Emory Users
