“Wound healing is a complex process requiring a finely tuned immune response. Cancer patients often have risk factors for impaired healing, including older age, malnutrition, steroid use, and prior treatments. Traditionally, oncologic therapies like cytotoxic chemotherapy or anti-angiogenic drugs (e.g., bevacizumab) are known to delay wound healing by suppressing cell proliferation or blood vessel growth. In contrast, immunotherapies stimulate immune activity rather than directly inhibiting regenerative pathways. The net effect of immunotherapy on wound repair is not yet fully understood. Early clinical observations have been mixed—some reports suggest immunotherapy can be given safely during the perioperative period, whereas others have noted higher rates of wound complications in certain settings. Given the increasing overlap of surgery, wound care, and immunotherapy in oncology, a thorough review of current evidence is warranted.”
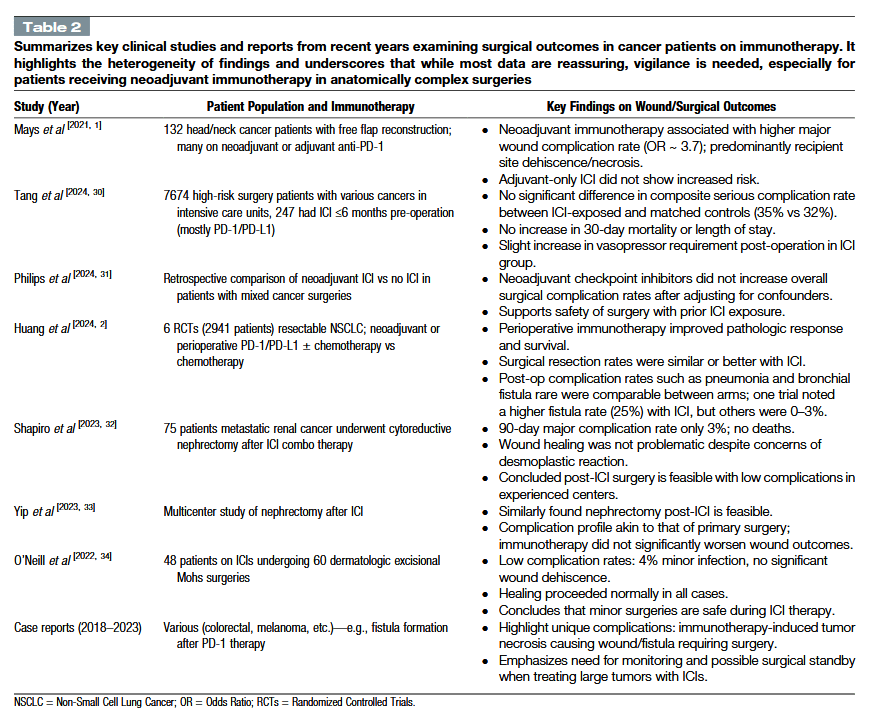
“Most cancer patients on immunotherapy heal surgical and accidental wounds without major issues. Large studies show no significant differences in surgical complication rates with ICIs.
However, immune system alterations can sometimes delay healing or cause unique wound pathologies. Neoadjuvant immunotherapy before complex surgeries has shown higher wound complication rates in some cohorts, suggesting careful patient selection is needed. Immune-related adverse effects can directly cause wounds (like autoimmune blistering diseases), requiring immunosuppressive treatment and specialized care. Clinicians
should watch impaired healing or unusual wound presentations. Early intervention—optimizing wound care, specialist consultation, or adjusting immunotherapy—prevents minor issues from becoming serious. A multidisciplinary approach involving oncologists, wound care specialists, and dermatologists is ideal. Patient education ensures prompt reporting of problems.”
Kuo, Pao-Jen et al. “Wound healing in cancer patients under immunotherapy.” International journal of surgery (London, England) vol. 111,10 (2025): 7087-7098.
