“Emergency general surgery (EGS) patients require greater resources and have increased rates of morbidity and mortality. Previous work has shown mortality differences in colectomy patients between direct admissions and transfers patients based on source, including emergency department, inpatient, and nursing home transfers. We hypothesize that patient transfer status negatively effects morbidity, mortality, and resource utilization in a mixed population of EGS patients.
This study demonstrates significant increases in mortality, morbidity, and resource utilization in EGS transfer patients who were not attributable to case mix, demographics, and comorbid status alone. These data point to potential financial and quality assessment challenges for tertiary referral centers.”
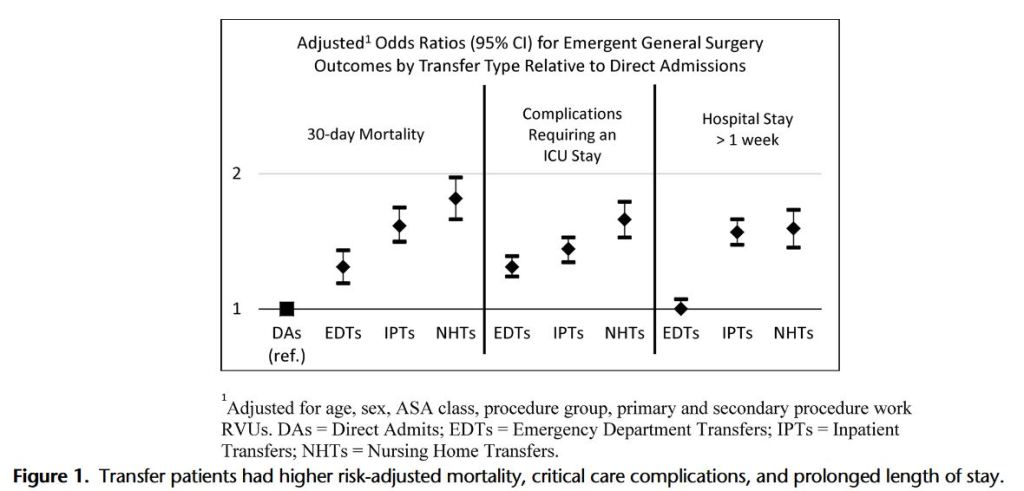
“This study demonstrates that transfer status has a significant impact on mortality, morbidity, and resource utilization in patients who have undergone EGS operations. Mortality of all transfer groups was significantly higher than DAs with NHTs having a mortality rate over 7 times that of DAs. There are many factors that may be driving this outcome difference between transfer groups. Delays to definitive treatment and source control increase acute physiological derangement, thus leading to more postoperative complications and mortality. Recent evidence has shown that the greatest risk factors for postoperative 30-day mortality are age, nonindependent functional status, preoperative sepsis, blood urea nitrogen level, and serum albumin level.”
Keeven DD, et al . Escalation of mortality and resource utilization in emergency general surgery transfer patients. J Trauma Acute Care Surg. 2019 Jul;87(1):43-48.
