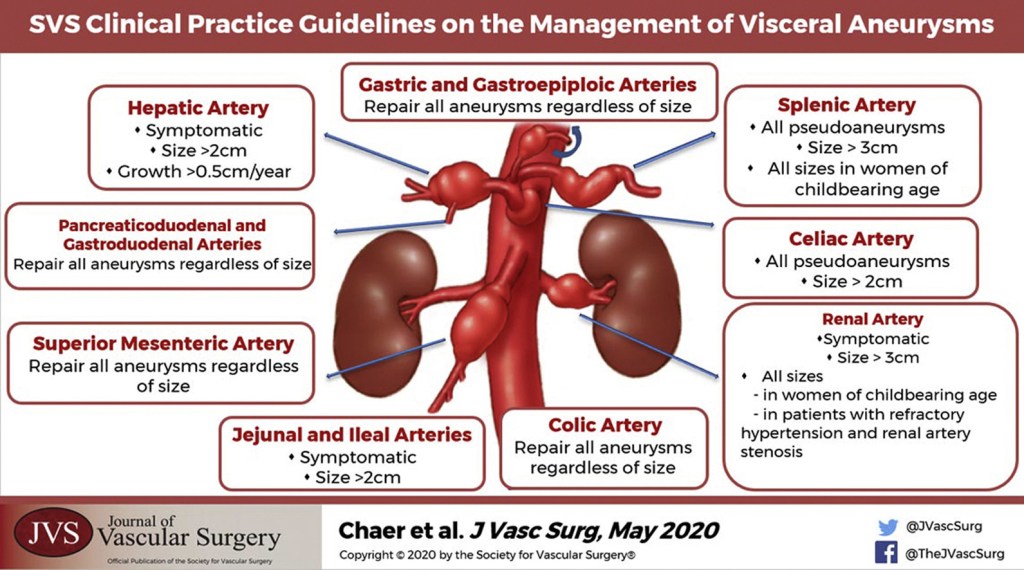
“Although not directed by randomized prospective trials, general principles of management of visceral artery aneurysms do exist. Because of their potential for rupture, most visceral artery pseudoaneurysms, mycotic aneurysms, and many larger true aneurysms warrant intervention. Treatment can generally be accomplished by either open surgical or endovascular approaches. The treatment goal is to prevent aneurysm expansion and potential rupture by exclusion from the arterial circulation while maintaining necessary distal or collateral bed perfusion. Depending on the location of the aneurysm, this can be accomplished in a variety of ways. In areas of the visceral circulation with an abundance of collateral flow, for example, in the splenic artery, proximal and distal ligation of the aneurysm segment is a viable surgical option. This can also be accomplished with endovascular isolation of the aneurysmal segment, either by placement of a stent graft or by coil embolization of the proximal and distal arterial segment. The preferred treatment of an individual patient and aneurysm must be carefully based on the particular anatomy and any associated clinical conditions as well as the underlying condition of the patient. The purpose of these guidelines is to inform the diagnosis, treatment options, screening, and follow-up of visceral aneurysms based on the available published literature and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach”
GRADE 1 Recommendations Summaries:
Renal artery aneurysm (RAA)
- In patients who are thought to have RAAs, we recommend computed tomography angiography (CTA) as the diagnostic tool of choice.
- In patients who are thought to have RAA and have increased radiation exposure risks or renal insufficiency, we recommend non-contrast-enhanced magnetic resonance angiography (MRA) to establish the diagnosis.
- We recommend the use of catheter-based angiography both for preoperative planning and to better delineate distal renal artery branches that may be inadequately assessed on conventional cross-sectional imaging.
- We recommend emergent intervention for any size RAA resulting in patient symptoms or rupture.
Splenic artery aneurysm (SAA)
- We recommend computed tomography angiography as the initial diagnostic tool of choice for SAAs.
- In patients with suspected SAAs and pre-existing renal insufficiency limiting the use of iodinated contrast material, we recommend magnetic resonance angiography to establish diagnosis.
- We recommend using arteriography when noninvasive studies have not sufficiently demonstrated the status of relevant collateral blood flow and when endovascular intervention is planned.
- We recommend emergent intervention for ruptured SAAs.
- We recommend treatment of nonruptured splenic artery pseudoaneurysms of any size in patients of acceptable risk because of the possibility of rupture.
- We recommend treating nonruptured splenic artery true aneurysms of any size in women of childbearing age because of the risk of rupture.
- We recommend treating nonruptured splenic artery true aneurysms >3 cm, with a demonstrable increase in size, or with associated symptoms in patients of acceptable risk because of the risk of rupture.
Celiac artery aneurysm (CAA)
- We recommend emergent intervention for ruptured CAAs.
- We recommend treatment of nonruptured celiac artery pseudoaneurysms of any size in patients of acceptable operative risk because of the possibility of rupture.
- We recommend treatment of nonruptured celiac artery true aneurysms >2 cm, with a demonstrable increase in size, or with associated symptoms in patients of acceptable risk because of the risk of rupture.
- In patients with ruptured CAA diagnosed on preoperative imaging studies who are stable, we recommend treatment with open surgical or appropriate endovascular methods based on the patient’s anatomy and underlying clinical condition.
Gastric and gastroepiploic artery aneurysms
- In patients who are thought to have gastric or gastroepiploic artery aneurysms, we recommend computed tomography angiography (CTA) as the diagnostic tool of choice.
- In patients who are thought to have gastric and gastroepiploic artery aneurysms and have high radiation exposure risks or renal insufficiency, we recommend non-contrast-enhanced magnetic resonance angiography (MRA) for diagnosis.
- We recommend the use of catheter-based angiography for all emergent cases presenting with rupture, and electively for preoperative planning
- We recommend treatment of all gastric artery and gastroepiploic artery aneurysms of any size.
- We recommend endovascular embolization for first-line treatment of gastric artery and gastroepiploic artery aneurysms.
Hepatic artery aneurysm (HAA)
- In patients who are thought to have HAA, we recommend computed tomography angiography (CTA) as the diagnostic tool of choice.
- In patients with HAA who are considered for intervention, we recommend mesenteric angiography for preoperative planning.
- Given the high propensity of rupture and significant antecedent mortality, we recommend that all hepatic artery pseudoaneurysms, regardless of cause, be repaired as soon as the diagnosis is made.
- We recommend repair of all symptomatic HAAs regardless of size.
- In asymptomatic patients without significant comorbidity, we recommend repair if true HAA is >2 cm, or if aneurysm enlarges >0.5 cm/y In patients with significant comorbidities, we recommend repair if HAA is >5.0 cm.
- We recommend repair of HAA in patients with vasculopathy or vasculitis, regardless of size,
- We recommend repair in HAA patients with positive blood cultures.
- We recommend an endovascular-first approach to all HAAs if it is anatomically feasible (ie, if this approach maintains arterial circulation to the liver).
- In patients with extrahepatic aneurysms, we recommend open and endovascular techniques to maintain liver circulation.
- In patients with intrahepatic aneurysms, we recommend coil embolization of the affected artery, In patients with large intrahepatic aneurysms, we recommend resection of the involved lobe of liver to avoid significant liver necrosis.
Superior mesenteric artery aneurysm (SMAA)
- In patients with SMAAs, we recommend computed tomography angiography (CTA) as the diagnostic tool of choice.
- We recommend mesenteric angiography to delineate anatomy in preoperative planning for SMAA repair.
- We recommend repair of all true SMAAs and pseudoaneurysms as soon as the diagnosis is made regardless of size.
- We recommend an endovascular-first approach to all SMAAs if it is anatomically feasible.
Jejunal, ileal, and colic artery aneurysms
- In patients who are thought to have jejunal artery, ileal artery, and colic artery aneurysms, we recommend computed tomography angiography (CTA) as the diagnostic tool of choice.
- In patients with high radiation exposure risks or renal insufficiency, we recommend non-contrast-enhanced magnetic resonance angiography (MRA) for diagnosis.
- We recommend the use of catheter-based angiography for all emergent cases presenting with rupture,and electively for preoperative planning,
- We recommend elective intervention for jejunal and ileal artery aneurysms >2 cm in maximal diameter and for all colic artery aneurysms, any size.
- We recommend emergent intervention for any jejunal, ileal, or colic artery aneurysm, any size, resulting in patient symptoms or rupture and all mesenteric branch vessel pseudoaneurysms
Pancreaticoduodenal artery aneurysm (PDAA) and gastroduodenal artery aneurysm (GDAA)
- In patients who are thought to have GDAA and PDAA, we recommend computed tomography angiography (CTA) as the diagnostic tool of choice.
- In patients with noncomplicated GDAA and PDAA of acceptable operative risk, we recommend treatment no matter the size of the aneurysm because of the risk of rupture.
- In patients with intact and ruptured aneurysms, we recommend coil embolization as the treatment of choice.
- In patients status post treatment of GDAA and PDAA, we recommend follow-up imaging after endovascular treatment of GDAA and PDAA to rule out persistent flow through the aneurysm sac.
Chaer, Rabih A et al. “The Society for Vascular Surgery clinical practice guidelines on the management of visceral aneurysms.” Journal of vascular surgery vol. 72,1S (2020): 3S-39S. Free Full Text.
