“Among patients with cancer, the estimated prevalence of malignancy-associated bowel
obstruction (MBO) is 3-15%, including up to 51% in ovarian cancer and up to 28% in
cancers of the gastrointestinal tract. MBO is among the most common palliative
indications for surgical consultation5 and typically signifies a poor prognosis, with mean
survival of 3-8 months in surgical cases and 4-5 weeks in those with inoperable MBO.
Managing the considerable symptom burden associated with MBO frequently
requires hospitalization and contributes to high-intensity healthcare utilization.1, In light
of national efforts to address the poor quality and high cost of care near the end of life, it is
critical to understand the relationship between treatment for complications of terminal
cancer, such as MBO, and end-of-life (EOL) care.”
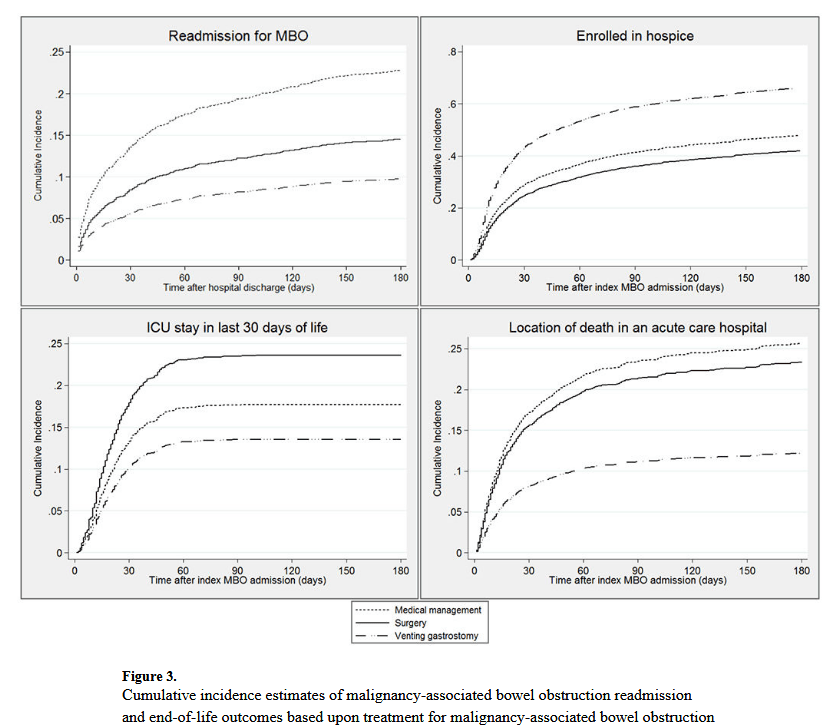
“The results of this study corroborate previous work demonstrating that MBO typically
occurs in the last months of life, with 65% of patients dying within 180 days of their first
MBO admission. In this population-based, retrospective cohort study of older Medicare
patients with MBO in the setting of ovarian or pancreatic cancer, the overall median survival
after the first MBO admission was less than 3 months, underscoring the relevance of EOL
care outcomes in delivering patient-centered care for these patients. Nonetheless, fewer than 5% had palliative care consultation. Patients treated with surgery at their first MBO
admission had the longest survival. Those treated with medical management had the highest rate of readmission for MBO. Treatment with VGT was associated with lower intensity healthcare utilization at the end of life than medical management or surgery.”
Lilley, Elizabeth J et al. “Survival, Healthcare Utilization, and End-of-life Care Among Older Adults With Malignancy-associated Bowel Obstruction: Comparative Study of Surgery, Venting Gastrostomy, or Medical Management.” Annals of surgery vol. 267,4 (2018): 692-699. Free Full Text
