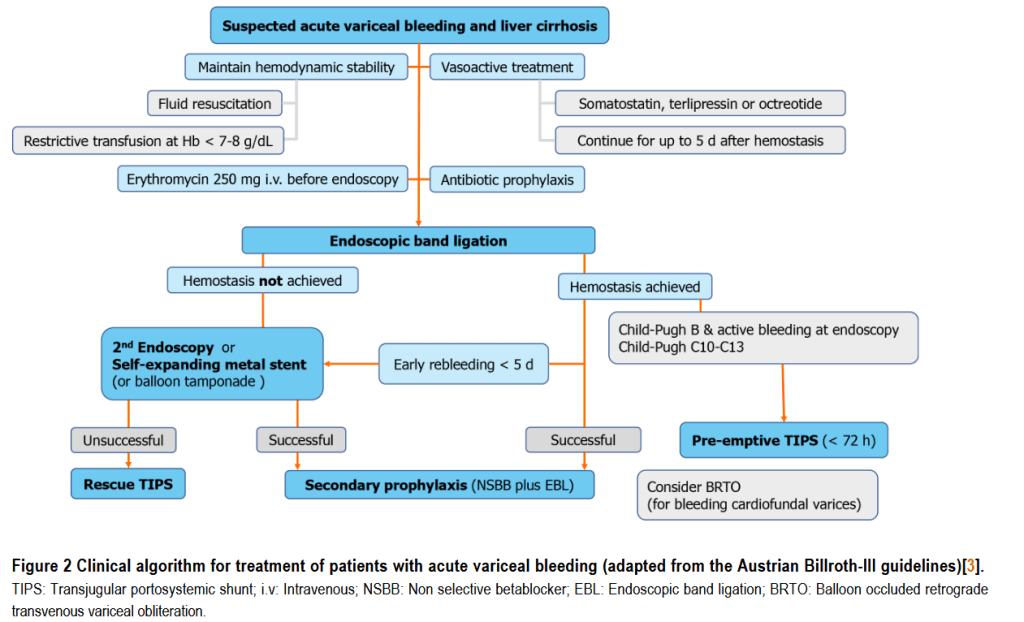
“Variceal bleeding is a severe, and often deadly, complication of portal hypertension. Screening for varices, effective bleeding prophylaxis and standardized management of bleeding is critical to improve clinical outcomes. While carvedilol seems to be the treatment of choice for primary prophylaxis in compensated cirrhosis, the use of hepatic venous pressure gradient measurements and safety of non-selective betablockers in advanced cirrhosis with refractory ascites is controversial. The pre-emptive use of transjugular intrahepatic portosystemic shunt within 72 h after variceal bleeding prevents rebleeding and mortality in Child C10-C13 patients.”
“In primary prophylaxis, NSBB or EBL are equal in outcomes and are therefore both
recommended as monotherapies to prevent a first variceal bleeding event.
However, carvedilol – due to its higher potency to lower portal pressure resulting
in higher proportions of HVPG responders – may be the treatment of choice for
primary prophylaxis in compensated cirrhosis. No clear recommendation for the use
of betablockers can be made for patients with small varices (even with additional risk
factors), as their efficacy in this setting remains unclear. Importantly, due to non-
hemodynamic effects of NSBBs on intestinal permeability, systemic inflammation
and considering the results of the recent PREDESCI trial showing reduced
risk of decompensation and mortality, NSBB may already be recommended for small
varices.
To monitor NSBB treatment response, invasive HVPG measurement is still
considered as gold standard, but other non-invasive surrogates to monitor NSBB
response to prevent variceal bleeding such as ultrasound-based elastography or
transient elastography assessment of the spleen are currently under consideration as
HVPG measurement is not widely available”
Pfisterer, Nikolaus et al. “Clinical algorithms for the prevention of variceal bleeding and rebleeding in patients with liver cirrhosis.” World journal of hepatology vol. 13,7 (2021): 731-746. doi:10.4254/wjh.v13.i7.731
