“Advances in surgical techniques and perioperative management over the last 2–3 decades have enabled the safe performance of hepatic resections. In the 1980s, when the perioperative mortality was reported to be as high as around 10%, drain placement was
considered to be necessary so as to provide information about intraabdominal adverse events promptly and for prophylactic drainage. However, as the necessity of drain placement in other surgical fields has been ruled out and as the incidence of life-threatening adverse
events after hepatic resection decreased, several randomized controlled trials (RCTs) were performed; the conclusions of these trials were that drain placement was not necessary. However, some of them lacked a primary endpoint and calculation of sample size; in
the other studies, the primary endpoint was the incidence of wound-related complication, most of which could be resolved using antibiotics or bed-side opening of the wound, corresponding to Clavien-Dindo (C-D) grade 11 2 or even 1.”
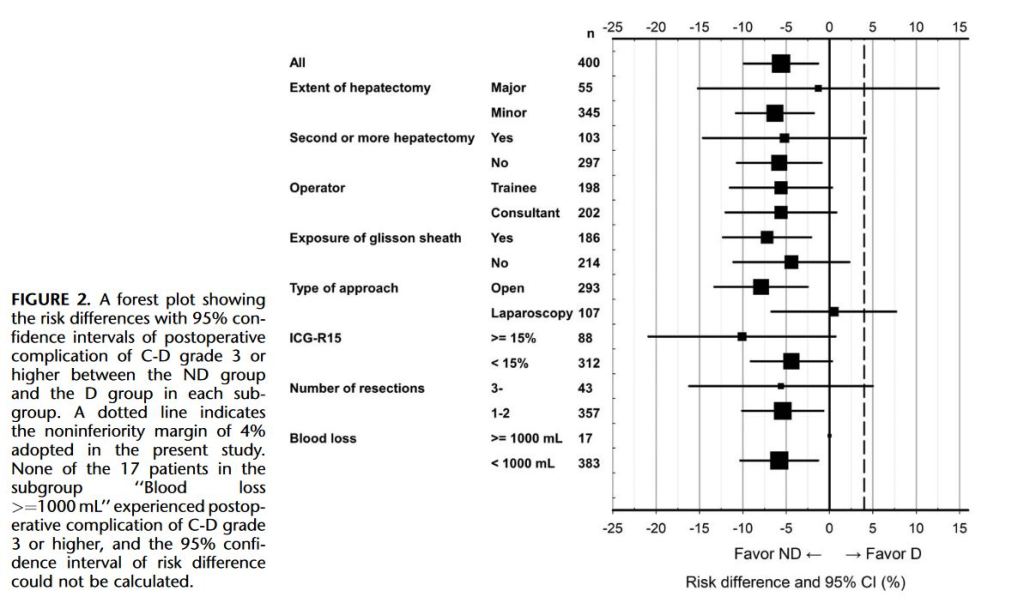
“This study has shown that drain placement increases the rate of severe postoperative complication in patients undergoing hepatic resection. To the best of our knowledge, this is the first RCT to assess the impact of drain placement after hepatic resection on the severe
postoperative complication rate classified according to C-D grading. The use of C-D grading enables assessment of short term results taking the clinical impact on patients into account. Furthermore, the present study used a strictly calculated sample size to confirm the study hypothesis.”
Arita J, et al Drain Placement After Uncomplicated Hepatic Resection Increases Severe Postoperative Complication Rate: A Japanese Multi-institutional Randomized Controlled Trial (ND-trial). Ann Surg. 2021 Feb 1;273(2):224-231.
