“Resections of the pancreas reaching to the left of the superior mesenteric vein are defined as distal pancreatectomy. Most distal pancreatectomies are done electively (84%) as a result of chronic pancreatitis (24%), other benign diseases (22%), malignant diseases (18%), neuroendocrine tumours (14%), and pancreatic pseudocysts (6%). The remaining 16% are emergency cases after abdominal trauma or miscellaneous pathological
diagnoses. A systematic review supports the evidence that postoperative pancreatic fistula formation represents a major source of postoperative morbidity (13–64%) and is associated with several further complications, such as intra-abdominal abscess, wound infection, sepsis, malabsorption, and haemorrhage.
A meta-analysis of the most favoured and reported techniques (stapler trans-section and closure vs scalpel trans-section and hand-sewn closure of the pancreatic remnant) did
not define the optimum surgical technique of pancreatic stump closure. Therefore, the multicentre randomised DISPACT trial was designed to assess the effect of stapler
versus hand-sewn closure on formation of postoperative pancreatic fistula after distal pancreatectomy.”
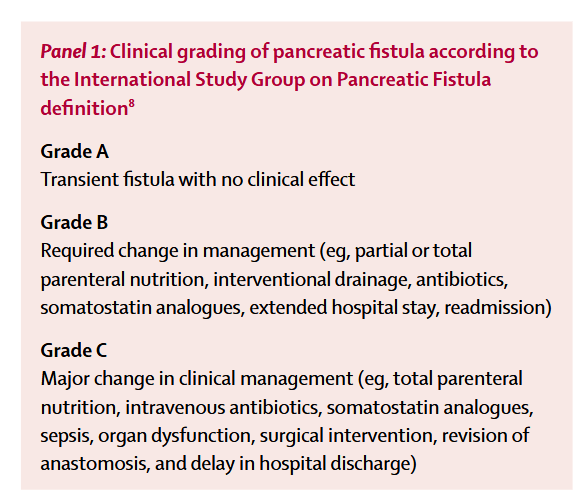
“Both stapler and hand-sewn closure were equally safe after distal pancreatectomy. The DISPACT trial did not show a reduction in postoperative pancreatic fistula and mortality up to postoperative day 7 by stapler resection and closure compared with scalpel resection and hand-sewn closure of the pancreatic remnant for distal pancreatectomy. Fistula formation therefore remains a clinically relevant and unsolved issue for patients undergoing distal pancreatectomy. Up to and including postoperative day 30, more than a third of patients have a pancreatic fistula after the procedure and a quarter have severe complications, according to the consensus classification. Occurrence of intra-abdominal fluid collection and abscesses were remarkably high (19% in both groups). Pancreatic fistula, intra-abdominal
collections, and abscesses often necessitate reintervention by interventional radiological-guided drainage, which itself increases hospital stay, comorbidity, pain, and discomfort for the affected patient. DISPACT showed that patients with pancreatic fistula had a mean extension of hospital stay of 6 days compared with those without fistula (mean 19·1 days vs 13·9 days), confirmed by multivariable analysis (p=0·037). Hospital stay in general is 5 days longer in Europe than in the USA.”
Diener, Markus K et al. “Efficacy of stapler versus hand-sewn closure after distal pancreatectomy (DISPACT): a randomised, controlled multicentre trial.” Lancet (London, England) vol. 377,9776 (2011): 1514-22. Emory Users Request via ILLiad
