One discussion this week focused on improving handoffs in the ICU.
Reference: Mukhopadhyay D, et al. Implementation of a standardized handoff protocol for post-opearative admissions to the surgical intensive care unit. American Journal of Surgery. 2018 Jan;215(1):28-36. doi:10.1016/j.amjsurg.2017.08.005.
Summary: Mukhopadhyay et al’s (2018) recent prospective intervention study explored the effectiveness of a standard protocol for patient transfer from the OR to the SICU. Prior to implementing a new protocol a team of individuals observed 31 patient handoffs. Next, the protocol was implemented over a 6 month period in which all caregivers involved in handoffs attended mandatory educational sessions. Finally, 31 handoffs were observed by the same team of individuals who had observed the previous handoffs.
Services included in the study: thoracic, neurosurgery, trauma, acute care, vascular, surgical oncology, urology, ENT, orthopedics, plastics, and neurointerventional radiology.
Handoff elements observed for completion: presence of all team-members at handoff; identification of patient and caregivers; detailed surgeon report; detailed anesthesia report; and duration/occurrence of key activities (time to ventilator, monitor set-up, total handoff duration).
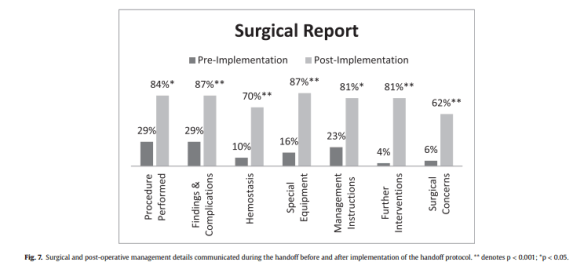
Results: Pre- and post-implementation performance was measured on all handoff elements listed above. These were elements identified as crucial to the safe and successful patient transfer.
Notably, surgeons were the only group that believed communication was effective in the existing process. Anesthesia and ICU Nursing were dissatisfied. All three groups agreed that a more structured protocol was necessary for safe patient care (p.29).
The figure below show the changes in degree of detail in surgical reports (p.35). The article provides additional charts and data on other pre- and post- findings.
Additional reading: Karamchandani K, et al. A multidisciplinary handoff process to standardize the transfer of care between the intensive care unit and the operating room. Quality Management in Health Care. 2018 Oct/Dec;27(4):215-222. doi:10.1097/QMH.0000000000000187.

