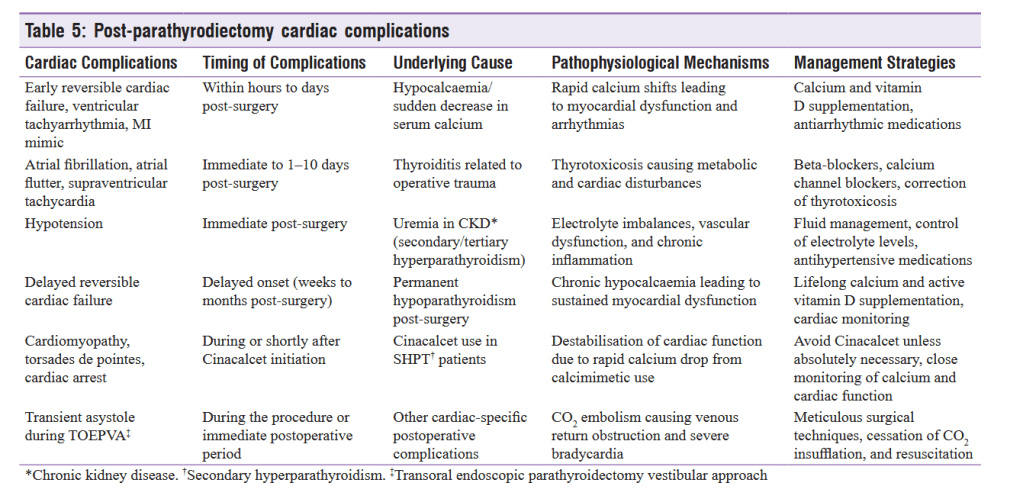
“Thyrotoxicosis has been reported as a postoperative complication of parathyroidectomy
(PTx), attributed to palpation thyroiditis. Palpation thyroiditis was first described by Carney et al., in 1975 as a pathologic response to the traumatic injury of thyroid follicles, characterized by multifocal granulomatous folliculitis. The existing cohort studies in post-PTx thyrotoxicosis are limited. A prospective study of patients who underwent PTx for primary and secondary HPT reported that the incidence rate of thyrotoxicosis after PTx was 31.2 % and 77 %, respectively. The clinical significance of post-PTx thyrotoxicosis remains controversial. While
various manifestations of thyrotoxicosis, including tremors, palpitations, new-onset atrial fibrillation, and angina pectoris mimicking myocardial infarction, were described by case reports, Stang et al. in a cohort study reported that only 15 % of patients developed symptoms of thyrotoxicosis 1–2 weeks after the operation. They further concluded
that the degree of neck dissection appeared explanatory but did not specify which maneuvers were contributory.”