“Air embolism is a rare but potentially fatal complication of surgical procedures. Rapid
recognition and intervention is critical for reducing morbidity and mortality.”
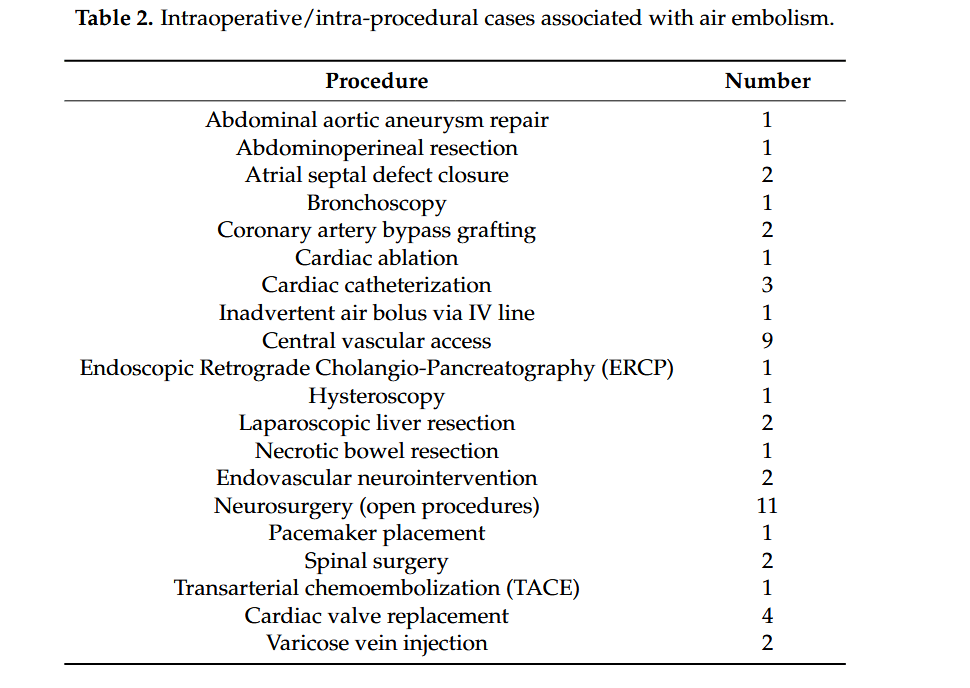
“Iatrogenic procedures are the main cause of vascular air embolism (VAE). This rare complication can arise in a wide range of clinical scenarios involving line placement, trauma, barotrauma, and several types of surgical procedures including cardiac, vascular, and neurosurgery. Traditionally, surgery and trauma were the most significant causes of systemic and cerebral air embolism; however, endoscopy, angiography, tissue biopsy, thoracocentesis, hemodialysis, and central/peripheral venous access now comprise a greater proportion. The insertion and maintenance of advanced vascular
access devices are increasingly being performed within multiple clinical specialties. Moreover, the bulk of interventional radiology (IR) procedures commence with the placement of an intravascular sheath, which is a major risk factor for air embolism throughout the duration of the procedure. Endovascular procedures complicated by an intravascular air embolism result in significant morbidity and mortality.
VAE is a potentially preventable condition, which arises as a result of a pressure gradient that allows air to enter the blood stream, which can subsequently cause blockages in blood flow. VAE has an estimated incidence of 1 in 772 according to one series, while another study found that the incidence of iatrogenic gas embolism complicates 2.65 per 100,000 hospitalizations; however, these figures are considered lower than the true incidence due to many unreported instances and undiagnosed asymptomatic patients.”