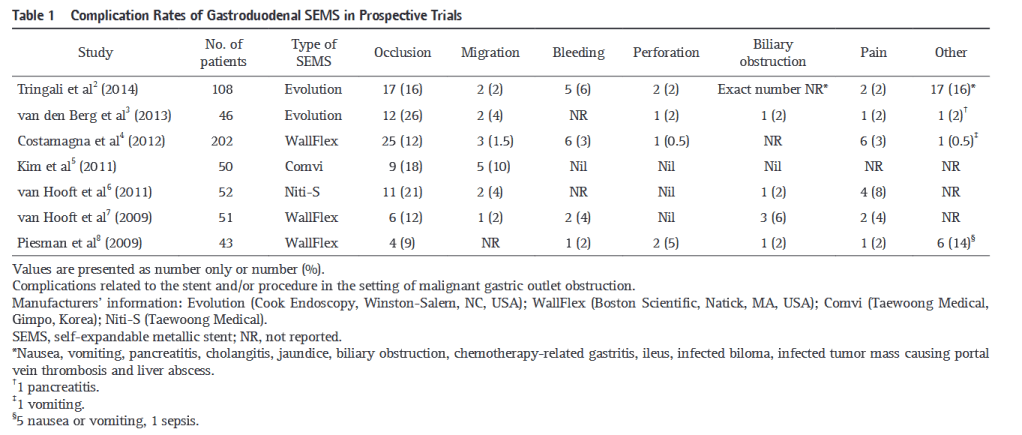
“Stent-related complications may be classified as early or late and major or minor. Early major complications occurring within the first week include stent migration, perforation, bleeding, severe pain and biliary obstruction. Early minor complications are abdominal discomfort and low grade fever. Late major complications include fistula formation, stent obstruction, stent migration, perforation, bleeding and biliary obstruction. Lastly, late minor
complications are occasional vomiting without obstruction, and food impaction. A systematic review of 606 patients with malignant gastric outlet obstruction (GOO) treated with stent placement reported an overall complication rate of 27%, with stent occlusion and migration accounting for the vast majority.”