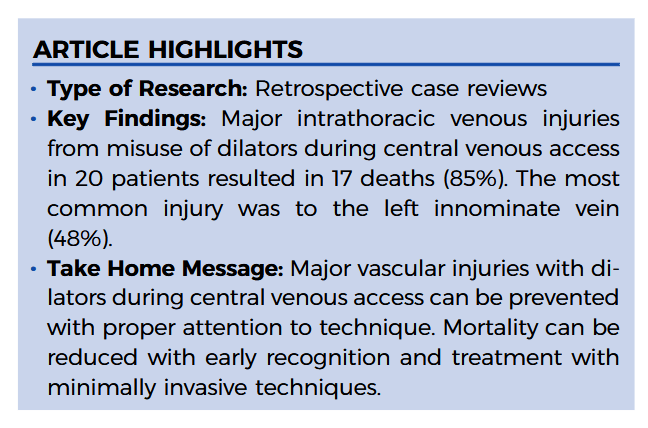
“Accessing central veins is a common procedure that is performed in many clinical settings. Complications are not infrequent events. Local complications have been reduced by the utilization of ultrasound guidance; however, this practice does not prevent injuries to the deep, intrathoracic veins.
Major venous injuries that occur within the thorax secondary to misuse of the dilator have been reported. The majority of these reports have been anecdotal case reports. There is very little evidence to suggest that a flexible, spring-loaded guidewire could perforate a
major vein. The dilator is the only instrument that has the stiffness and point that is capable of perforating a central vein.”