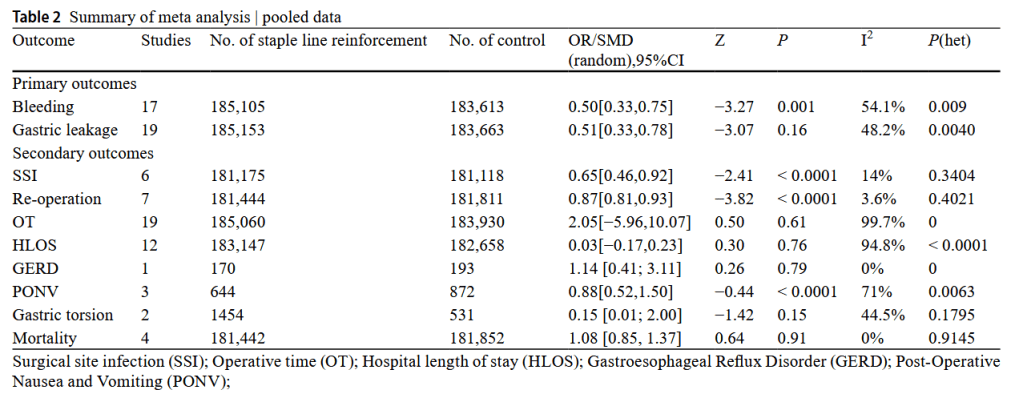
“The efficacy of bariatric surgery in facilitating sustained weight loss and managing obesity-related comorbidities has been consistently reported in the medical/scientific literature. Sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) are widely accepted bariatric procedures. However, complications, such as gastric leakage, bleeding, stricture, and surgical infection, can lead to significant morbidity and mortality, posing a formidable challenge to bariatric surgeons.
In order to reduce the incidence of complications associated with bariatric surgery, some surgeons have advocated the use of gastric incision staple line reinforcement with the
aim of improving structural integrity and reducing edge tension. However, others have suggested that the reinforcement of the incision edge may compromise suture stability, thereby raising concerns about the overall effectiveness of staple line reinforcement in preventing postoperative complications.”