“There is evidence of endothelial dysfunction and a dysregulation of coagulation and fibrinolysis in individuals with HIV. In a study of 109 HIV-infected patients with advanced disease, 10% developed venous thrombosis and 6% developed arterial thrombosis. A variety of laboratory abnormalities were reported, including protein C deficiency, increased factor VIII concentrations, high fibrinogen concentrations, and free protein S deficiency. HIV infection is also associated with an increased D-dimer level, which suggests that HIV infection might be associated with a pro-thrombotic state. HIV disease is theorized to produce a pro-thrombotic state through mechanisms related to activation of the innate and adaptive immune system by low level HIV replication, co-pathogens, and microbial products trans-located from the gastrointestinal tract,”
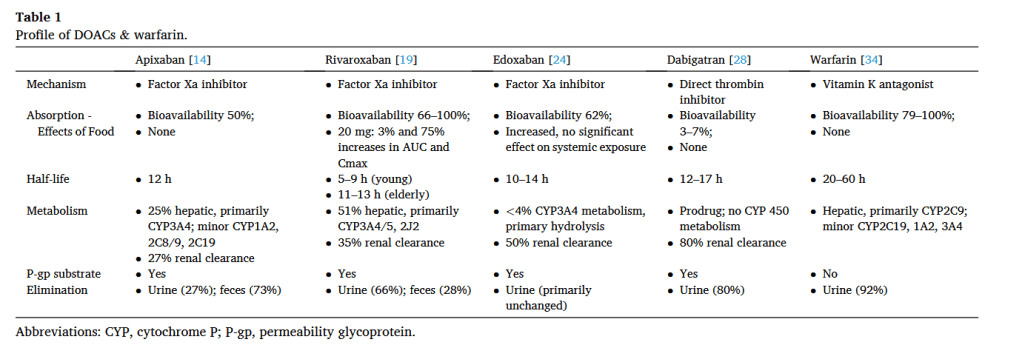
“The impact of HAART on coagulation is unclear. Protease inhibitors (PI) have been associated with higher fibrinogen levels and lipodystrophy. PIs are also thought to interfere with cytochrome P (CYP) 450 metabolism and regulation of thrombotic proteins. This may
cause a pro-thrombotic state in HIV-infected individuals”