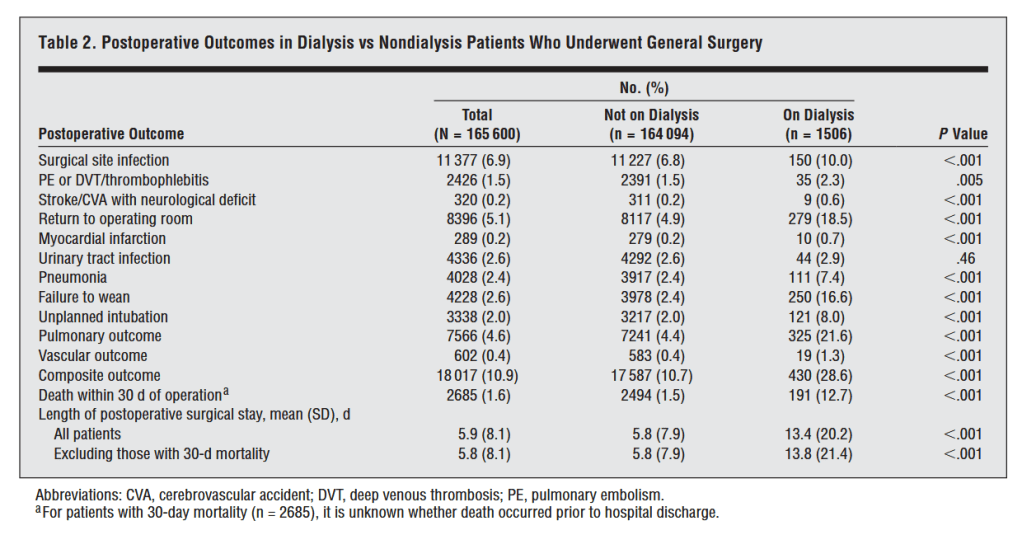
“More than half a million individuals in the United States undergo dialysis, a number that has been forecasted to increase by 7% annually. End-stage renal disease requiring dialysis is associated with poor health care outcomes, including a 10-fold increase in risk of hospitalization and an expected lifespan between one-fourth and one-sixth of that of the general population. Despite the well-described outcomes of the effect of end-stage renal disease on community-dwelling individuals, little is known about the contribution of long-term dialysis to the risks of postoperative complications and death.”