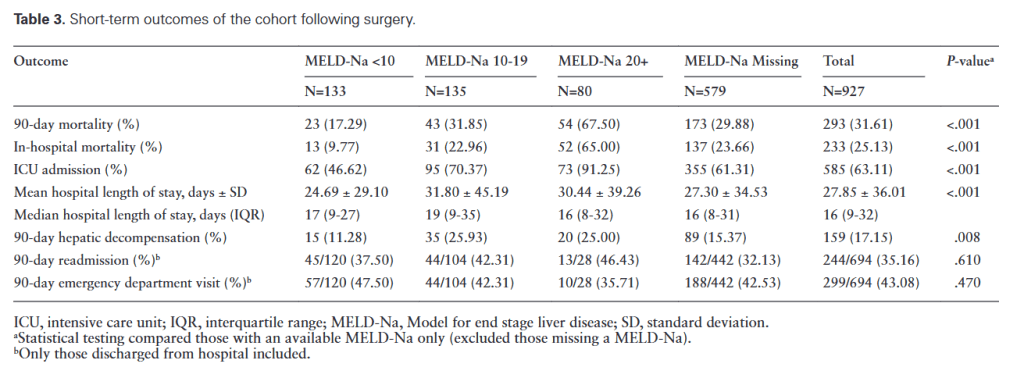
“Individuals with cirrhosis have higher post-operative morbidity and mortality following major abdominal surgery compared to those without cirrhosis. To quantify this added risk, observational studies and prediction models have been described; however, the majority were derived from historic cohorts and may not reflect the changing epidemiology of
liver disease or advances in both the medical management of cirrhosis and perioperative practices in this high-risk group.”