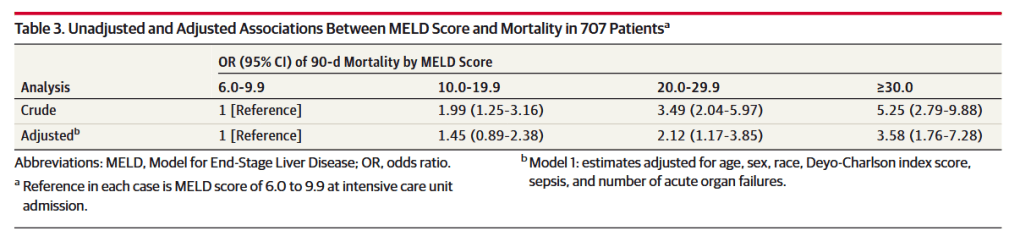
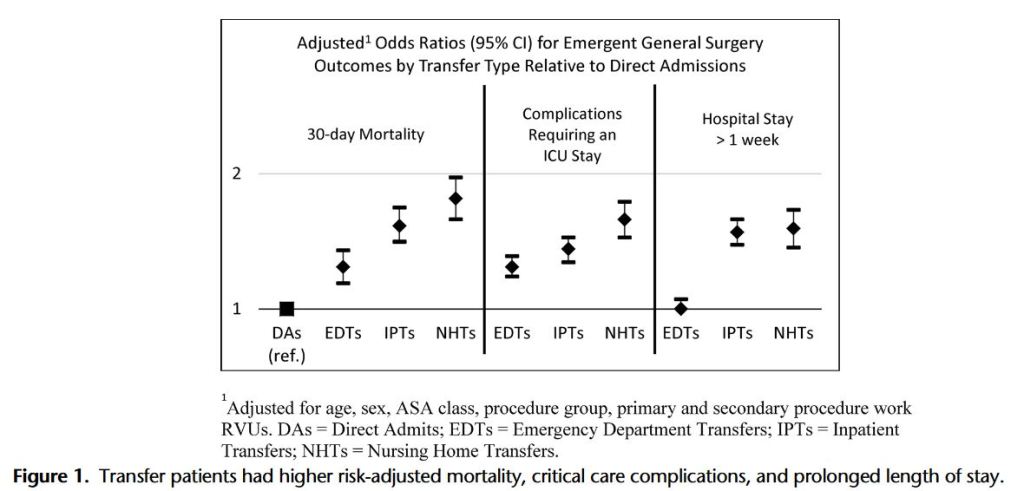
“Emergency general surgery (EGS) is associated with increased rates of morbidity and mortality compared with non-emergent general surgery cases.8 Patients undergoing EGS are approximately 2.5 times more likely to experience a significant complication and have a 6-fold increase in mortality relative to non-EGS patients. The underlying causes of this increased morbidity and mortality are not fully understood, but medical comorbidities and physiological derangements are likely to be contributing factors. Although surgical risk calculation tools such as the American College of Surgeons National Surgical Quality Improvement Project Surgical Risk Calculator are used to gain an objective sense of surgical risk stratification, such tools have yet to be comprehensively studied in this patient population and do not include the use of liver disease–specific assessment tools such as the MELD score in the prediction of outcomes among patients with CLD undergoing EGS.”