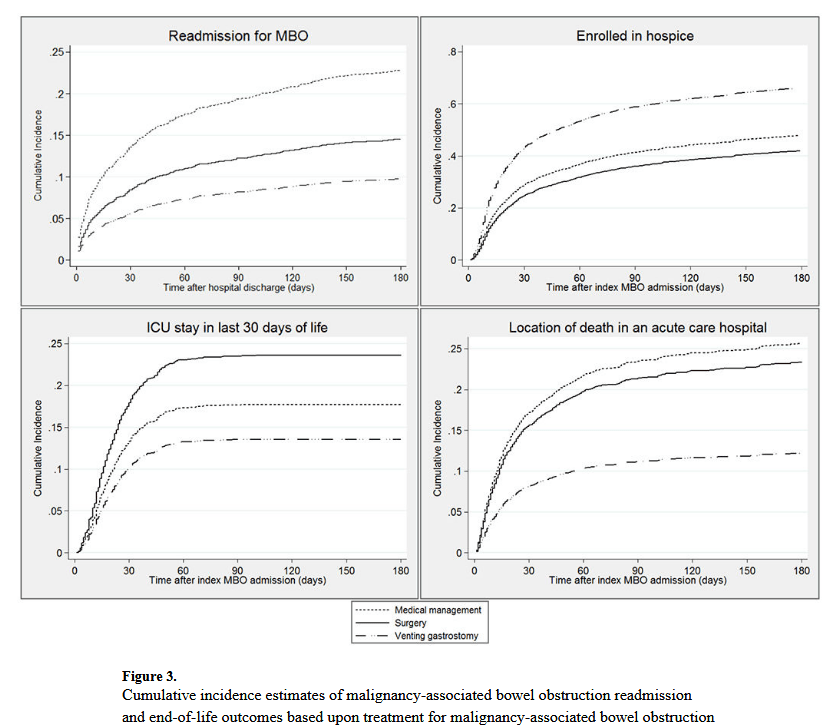
“Among patients with cancer, the estimated prevalence of malignancy-associated bowel
obstruction (MBO) is 3-15%, including up to 51% in ovarian cancer and up to 28% in
cancers of the gastrointestinal tract. MBO is among the most common palliative
indications for surgical consultation5 and typically signifies a poor prognosis, with mean
survival of 3-8 months in surgical cases and 4-5 weeks in those with inoperable MBO.
Managing the considerable symptom burden associated with MBO frequently
requires hospitalization and contributes to high-intensity healthcare utilization.1, In light
of national efforts to address the poor quality and high cost of care near the end of life, it is
critical to understand the relationship between treatment for complications of terminal
cancer, such as MBO, and end-of-life (EOL) care.”