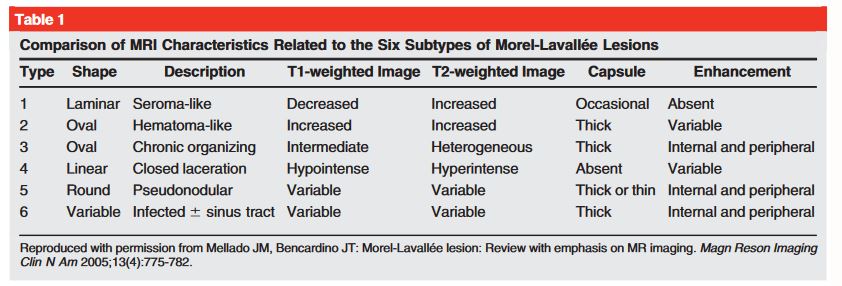
“The Morel-Lavallee lesion clinically presents as a painful fluctuant swelling at the site of involvement. Concerning the recent literature available, this lesion is also termed as Morel-Lavallée seroma, posttraumatic soft tissue cyst, post-traumatic extravasation, or Morel-Lavallée effusion. This lesion may be missed at the time of initial assessment and can present later, potentially leading to increasing difficulty in management and long-term morbidity.”
“The most common causes of Morel-Lavallee lesions are high-velocity trauma, crush injuries, and blunt trauma. Overall, approximately twenty-five percent of all patients who develop Morel-Lavallee lesions have been involved in a road traffic accident. This lesion is commonly associated with underlying fractures, especially of the proximal femur, pelvis, and acetabulum. One of the most commonly involved regions is the greater trochanter, accounting for more than sixty percent of the cases”
Continue reading →