| Topic | Articles |
| Gallbladder | |
| Appendicitis | Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986 May;15(5):557-64. doi: 10.1016/s0196-0644(86)80993-3. PMID: 3963537. CODA Collaborative, Flum DR, Davidson GH, et al. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N Engl J Med. 2020 Nov 12;383(20):1907-1919. doi: 10.1056/NEJMoa2014320. PMID: 33017106. St Peter SD, et al. Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg. 2012 Oct;256(4):581-5. doi: 10.1097/SLA.0b013e31826a91e5. PMID: 22964730. Salminen P, Tuominen R, Paajanen H, et al. Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial. JAMA. 2018 Sep 25;320(12):1259-1265. doi: 10.1001/jama.2018.13201. PMID: 30264120; PMCID: PMC6233612. Sawyer RG, et al.; STOP-IT Trial Investigators. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015 May 21;372(21):1996-2005. doi: 10.1056/NEJMoa1411162. Erratum in: N Engl J Med. 2018 Jan 25. PMID: 25992746; PMCID: PMC4469182. |
| Peptic Ulcer Disease | Burch JM, Cox CL, Feliciano DV, Richardson RJ, Martin RR. Management of the difficult duodenal stump. Am J Surg. 1991 Dec;162(6):522-6. doi: 10.1016/0002-9610(91)90102-j. PMID: 1670218. |
| Cholelithiasis | Hunter JG. Avoidance of bile duct injury during laparoscopic cholecystectomy. Am J Surg. 1991 Jul;162(1):71-6. doi: 10.1016/0002-9610(91)90207-t. PMID: 1829588. Strasberg SM. Avoidance of biliary injury during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2002;9(5):543-7. doi: 10.1007/s005340200071. PMID: 12541037. |
| Intra-abdominal Infection | Guidry CA, Sawyer RG. Short-Course Antimicrobial Therapy for Intraabdominal Infection. N Engl J Med. 2015 Oct 15;373(16):1578. doi: 10.1056/NEJMc1508694. PMID: 26466002; PMCID: PMC4699292. Saunte DML, Jemec GBE. Hidradenitis Suppurativa: Advances in Diagnosis and Treatment. JAMA. 2017 Nov 28;318(20):2019-2032. doi: 10.1001/jama.2017.16691. PMID: 29183082. |
| Pancreatitis | Bergman S, Melvin WS. Operative and nonoperative management of pancreatic pseudocysts. Surg Clin North Am. 2007 Dec;87(6):1447-60, ix. doi: 10.1016/j.suc.2007.09.003. PMID: 18053841. Besselink MG, van Santvoort HC, Nieuwenhuijs VB, et al.; Dutch Acute Pancreatitis Study Group. Minimally invasive ‘step-up approach’ versus maximal necrosectomy in patients with acute necrotising pancreatitis (PANTER trial): design and rationale of a randomised controlled multicenter trial [ISRCTN13975868]. BMC Surg. 2006 Apr 11;6:6. doi: 10.1186/1471-2482-6-6. PMID: 16606471; PMCID: PMC1508161. Boerma D, et al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet. 2002 Sep 7;360(9335):761-5. doi: 10.1016/S0140-6736(02)09896-3. PMID: 12241833. Boxhoorn L, et al. Acute pancreatitis. Lancet. 2020 Sep 5;396(10252):726-734. doi: 10.1016/S0140-6736(20)31310-6. Erratum in: Lancet. 2021 Nov 6;398(10312):1686. PMID: 32891214. Branum G, Galloway J, Hirchowitz W, Fendley M, Hunter J. Pancreatic necrosis: results of necrosectomy, packing, and ultimate closure over drains. Ann Surg. 1998 Jun;227(6):870-7. doi: 10.1097/00000658-199806000-00010. PMID: 9637550; PMCID: PMC1191394. Kao LS, McCauley JS. Evidence-Based Management of Gallstone Pancreatitis. Adv Surg. 2020 Sep;54:173-189. doi: 10.1016/j.yasu.2020.04.005. PMID: 32713429. Van Buren G 2nd, Vollmer CM Jr. The Landmark Series: Mitigation of the Postoperative Pancreatic Fistula. Ann Surg Oncol. 2021 Feb;28(2):1052-1059. |
COLORECTAL SURGERY
HEPATOBILIARY SURGERY
| Topic | Articles |
| Gallbladder Cancer | Butte JM, et al. Residual disease predicts outcomes after definitive resection for incidental gallbladder cancer. J Am Coll Surg. 2014 Sep;219(3):416-29. doi: 10.1016/j.jamcollsurg.2014.01.069. PMID: 25087941. D’Angelica M, et al. Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann Surg Oncol. 2009 Apr;16(4):806-16. doi: 10.1245/s10434-008-0189-3. PMID: 18985272. Ethun CG, Postlewait LM, Le N, Pawlik TM, Buettner S, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Jin LX, Weber SM, Salem A, Martin RC, Scoggins C, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Merchant N, Cardona K, Maithel SK. A Novel Pathology-Based Preoperative Risk Score to Predict Locoregional Residual and Distant Disease and Survival for Incidental Gallbladder Cancer: A 10-Institution Study from the U.S. Extrahepatic Biliary Malignancy Consortium. Ann Surg Oncol. 2017 May;24(5):1343-1350. doi: 10.1245/s10434-016-5637-x. PMID: 27812827. Ethun CG, Postlewait LM, Le N, Pawlik TM, Buettner S, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Jin LX, Weber SM, Salem A, Martin RC, Scoggins C, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Kooby DA, Maithel SK. Association of Optimal Time Interval to Re-resection for Incidental Gallbladder Cancer With Overall Survival: A Multi-Institution Analysis From the US Extrahepatic Biliary Malignancy Consortium. JAMA Surg. 2017 Feb 1;152(2):143-149. doi: 10.1001/jamasurg.2016.3642. PMID: 27784058. Ethun CG, Postlewait LM, Le N, Pawlik TM, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Krasnick BA, Weber SM, Salem A, Martin RCG, Scoggins CR, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Cardona K, Maithel SK. Routine port-site excision in incidentally discovered gallbladder cancer is not associated with improved survival: A multi-institution analysis from the US Extrahepatic Biliary Malignancy Consortium. J Surg Oncol. 2017 Jun;115(7):805-811. doi: 10.1002/jso.24591. PMID: 28230242. Gamboa AC, Maithel SK. The Landmark Series: Gallbladder Cancer. Ann Surg Oncol. 2020 Aug;27(8):2846-2858. Primrose JN, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019 May;20(5):663-673. doi: 10.1016/S1470-2045(18)30915-X. Epub 2019 Mar 25. Erratum in: Lancet Oncol. 2019 Apr 2;: PMID: 30922733. |
| Cholangiocarcinoma | Brindley PJ, et al. Cholangiocarcinoma. Nat Rev Dis Primers. 2021 Sep 9;7(1):65. doi: 10.1038/s41572-021-00300-2. PMID: 34504109. Cloyd JM, Ejaz A, Pawlik TM. The Landmark Series: Intrahepatic Cholangiocarcinoma. Ann Surg Oncol. 2020 Aug;27(8):2859-2865. Maithel SK, Gamblin TC, Kamel I, Corona-Villalobos CP, Thomas M, Pawlik TM. Multidisciplinary approaches to intrahepatic cholangiocarcinoma. Cancer. 2013 Nov 15;119(22):3929-42. doi: 10.1002/cncr.28312. PMID: 23963845. Rea DJ, et al. Liver transplantation with neoadjuvant chemoradiation is more effective than resection for hilar cholangiocarcinoma. Ann Surg. 2005 Sep;242(3):451-8; discussion 458-61. doi: 10.1097/01.sla.0000179678.13285.fa. PMID: 16135931. Rocha FG, et al. Hilar cholangiocarcinoma: the Memorial Sloan-Kettering Cancer Center experience. J Hepatobiliary Pancreat Sci. 2010 Jul;17(4):490-6. doi: 10.1007/s00534-009-0205-4. PMID: 19806295. Soares KC, Jarnagin WR. The Landmark Series: Hilar Cholangiocarcinoma. Ann Surg Oncol. 2021 Aug;28(8):4158-4170. doi: 10.1245/s10434-021-09871-6. PMID: 33829358; PMCID: PMC9273057. Tao R, et al. Ablative Radiotherapy Doses Lead to a Substantial Prolongation of Survival in Patients With Inoperable Intrahepatic Cholangiocarcinoma: A Retrospective Dose Response Analysis. J Clin Oncol. 2016 Jan 20;34(3):219-26. doi: 10.1200/JCO.2015.61.3778. Erratum in: J Clin Oncol. 2019 Apr 10;37(11):942. PMID: 26503201. |
| Benign Liver Tumors | |
| Hepatocellular Carcinoma | Cheng AL, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009 Jan;10(1):25-34. doi: 10.1016/S1470-2045(08)70285-7. PMID: 19095497. Finn RS, et al.; IMbrave150 Investigators. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020 May 14;382(20):1894-1905. doi: 10.1056/NEJMoa1915745. PMID: 32402160. Llovet JM, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021 Jan 21;7(1):6. doi: 10.1038/s41572-020-00240-3. PMID: 33479224. Llovet JM, et al.; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008 Jul 24;359(4):378-90. doi: 10.1056/NEJMoa0708857. PMID: 18650514. Mazzaferro V, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996 Mar 14;334(11):693-9. doi: 10.1056/NEJM199603143341104. PMID: 8594428. |
| Liver Metastases | Gangi A, Howe JR. The Landmark Series: Neuroendocrine Tumor Liver Metastases. Ann Surg Oncol. 2020 Sep;27(9):3270-3280. doi: 10.1245/s10434-020-08787-x. PMID: 32632880; PMCID: PMC7415723. Kawaguchi Y, Vauthey JN. The Landmark Series: RCTs Examining Perioperative Chemotherapy and Postoperative Adjuvant Chemotherapy for Resectable Colorectal Liver Metastasis. Ann Surg Oncol. 2020 Oct;27(11):4263-4270. doi: 10.1245/s10434-020-08809-8. PMID: 32642998. |
| Pancreatic Adenocarcinoma | Dillhoff M, Pawlik TM. Role of Node Dissection in Pancreatic Tumor Resection. Ann Surg Oncol. 2021 Apr;28(4):2374-2381. See also: ASO Author Reflections: Role of Node Dissection in Pancreatic Tumor Resection. He J, et al. Landmark Series: Neoadjuvant Treatment in Borderline Resectable Pancreatic Cancer. Ann Surg Oncol. 2021 Mar;28(3):1514-1520. Rocha FG. Landmark Series: Immunotherapy and Targeted Therapy for Pancreatic Cancer. Ann Surg Oncol. 2021 Mar;28(3):1400-1406. doi: 10.1245/s10434-020-09367-9. PMID: 33386541. Sachs TE, Tseng JF. Landmark Series in Pancreatic Tumors: Anastomotic Techniques and Route of Reconstruction. Ann Surg Oncol. 2021 Apr;28(4):2227-2234. Shah MM, Datta J, Merchant NB, Kooby DA. Landmark Series: Importance of Pancreatic Resection Margins. Ann Surg Oncol. 2022 Mar;29(3):1542-1550. doi: 10.1245/s10434-021-11168-7. PMID: 34985731. van Hilst J, et al. The Landmark Series: Minimally Invasive Pancreatic Resection. Ann Surg Oncol. 2021 Mar;28(3):1447-1456. doi: 10.1245/s10434-020-09335-3. PMID: 33341916; PMCID: PMC7892688. White RR, Murphy JD, Martin RCG. The Landmark Series: Locally Advanced Pancreatic Cancer and Ablative Therapy Options. Ann Surg Oncol. 2021 Aug;28(8):4173-4180. |
| Non-PDAC Masses of the Pancreas | Tanaka M, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017 Sep-Oct;17(5):738-753. doi: 10.1016/j.pan.2017.07.007. PMID: 28735806. |
| Chronic Pancreatitis | |
| Bile Duct Injury | |
| Choledochal Cysts | |
| Gastric Cancer | Al-Batran SE, et al.; FLOT4-AIO Investigators. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet. 2019 May 11;393(10184):1948-1957. doi: 10.1016/S0140-6736(18)32557-1. PMID: 30982686. Cunningham D, et al., MAGIC Trial Participants. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006 Jul 6;355(1):11-20. doi: 10.1056/NEJMoa055531. PMID: 16822992. Dineen SP, Pimiento JM. The Landmark Series: Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (CRS/HIPEC) for Treatment of Gastric Cancer Metastatic to Peritoneum. Ann Surg Oncol. 2021 Aug;28(8):4130-4137. Ng SP, Leong T. Role of Radiation Therapy in Gastric Cancer. Ann Surg Oncol. 2021 Aug;28(8):4151-4157. |
| GIST | Keung EZ, et al. The Landmark Series: Systemic Therapy for Resectable Gastrointestinal Stromal Tumors. Ann Surg Oncol. 2020 Oct;27(10):3659-3671. |
EUH SURGERY B/EUHM/ ESJH GENERAL SURGERY
EUH Surgery A
| TOPIC | ARTICLES |
| Portal HTN | Millikan WJ Jr, et al. The Emory prospective randomized trial: selective versus nonselective shunt to control variceal bleeding. Ten year follow-up. Ann Surg. 1985 Jun;201(6):712-22. doi: 10.1097/00000658-198506000-00007. PMID: 3890781; PMCID: PMC1250801. Salam AA, et al. Hemodynamic contrasts between selective and total portal-systemic decompression. Ann Surg. 1971 May;173(5):827-44. doi: 10.1097/00000658-197105000-00022. PMID: 4933303; PMCID: PMC1397510. Wong M, Busuttil RW. Surgery in Patients with Portal Hypertension. Clin Liver Dis. 2019 Nov;23(4):755-780. doi: 10.1016/j.cld.2019.07.003. PMID: 31563221. |
| Non-HPB Cirrhosis General Surgery | Endale Simegn A, et al. Perioperative management of patients with liver disease for non-hepatic surgery: A systematic review. Ann Med Surg (Lond). 2022 Feb 24;75:103397. doi: 10.1016/j.amsu.2022.103397. PMID: 35242334; PMCID: PMC8886011. Johnson KM, et al. Incidence and Risk Factors of Postoperative Mortality and Morbidity After Elective Versus Emergent Abdominal Surgery in a National Sample of 8193 Patients With Cirrhosis. Ann Surg. 2021 Oct 1;274(4):e345-e354. doi: 10.1097/SLA.0000000000003674. PMID: 31714310. Neeff HP, et al. Early mortality and long-term survival after abdominal surgery in patients with liver cirrhosis. Surgery. 2014 Apr;155(4):623-32. doi: 10.1016/j.surg.2013.11.009. PMID: 24468037. Theruvath TP, Adams DB. Preoperative transjugular intrahepatic portosystemic shunt for extrahepatic surgery in cirrhosis. Am Surg. 2010 Jan;76(1):115-7. PMID: 20135955. |
| ECF & Surgical Nutrition | Boullata JI, et al. ASPEN Safe Practices for Enteral Nutrition Therapy [Formula: see text]. JPEN J Parenter Enteral Nutr. 2017 Jan;41(1):15-103. doi: 10.1177/0148607116673053. PMID: 27815525. Compher C, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr. 2022 Jan;46(1):12-41. doi: 10.1002/jpen.2267. Erratum in: JPEN J Parenter Enteral Nutr. 2022 Jun 19;: PMID: 34784064. Owen RM, Love TP, Perez SD, Srinivasan JK, Sharma J, Pollock JD, Haack CI, Sweeney JF, Galloway JR. Definitive surgical treatment of enterocutaneous fistula: outcomes of a 23-year experience. JAMA Surg. 2013 Feb;148(2):118-26. doi: 10.1001/2013.jamasurg.153. PMID: 23560282 |
| Inflammatory Bowel Disease | Ban KA, et al. Effect of Diagnosis on Outcomes in the Setting of Enhanced Recovery Protocols. Dis Colon Rectum. 2018 Jul;61(7):847-853. doi: 10.1097/DCR.0000000000001102. PMID: 29878952. Braga Neto MB, et al. Impact of Bariatric Surgery on the Long-term Disease Course of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2020 Jun 18;26(7):1089-1097. doi: 10.1093/ibd/izz236. PMID: 31613968; PMCID: PMC7534455. Hanauer SB, et al.; ACCENT I Study Group. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002 May 4;359(9317):1541-9. doi: 10.1016/S0140-6736(02)08512-4. PMID: 12047962. Lowe SC, et al. Declining Rates of Surgery for Inflammatory Bowel Disease in the Era of Biologic Therapy. J Gastrointest Surg. 2021 Jan;25(1):211-219. doi: 10.1007/s11605-020-04832-y. PMID: 33140318. Kline BP, et al. Clinical and Genetic Factors Impact Time to Surgical Recurrence After Ileocolectomy for Crohn’s Disease. Ann Surg. 2021 Aug 1;274(2):346-351. doi: 10.1097/SLA.0000000000003660. PMID: 31714311. Myrelid P, Kalman TD. Old, New, and Out of the Box in IBD Surgery: Proceedings of the European Crohn’s and Colitis Organisation 2020 Congress from a Surgical Perspective. Dis Colon Rectum. 2021 Aug 1;64(8):929-931. doi: 10.1097/DCR.0000000000002102. PMID: 33872289 Reinisch W, et al. Long-term infliximab maintenance therapy for ulcerative colitis: the ACT-1 and -2 extension studies. Inflamm Bowel Dis. 2012 Feb;18(2):201-11. doi: 10.1002/ibd.21697. PMID: 21484965. |
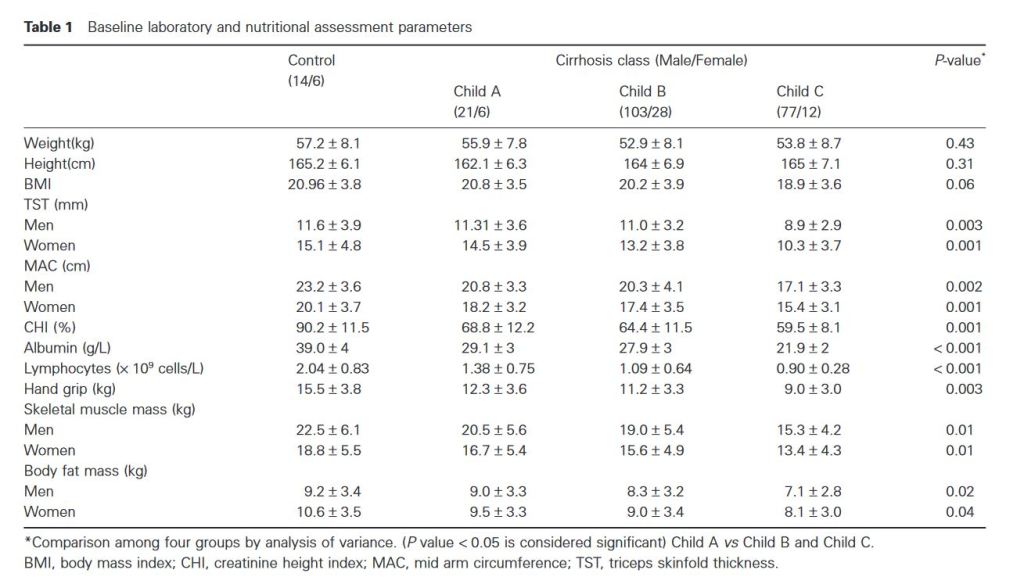
Cirrhotic nutritional management
“Prevalence of malnutrition in chronic liver disease ranges between 10% and 100%, depends on severity of liver disease. Prevalence is more in patients with alcoholic cirrhosis compared to nonalcoholic cirrhotics. 3 Malnutrition is seen in all clinical stages but is easier to detect in advanced stages of liver cirrhosis. Many patients have subtle changes such as fat soluble vitamin deficiency, anemia from iron, folate or pyridoxine deficiency, altered cell-mediated immune functions and minimal loss of muscle mass, while patients with end-stage liver disease have muscle wasting, decreased fat stores, and cachexia.”
Vascular injury in hernia repair
“Complications are known to occur at each and every step of hernia surgery. Applying caution while performing each step can save the patient from a lot of morbidity. One starts by applying strict patient selection criteria for endoscopic hernia repair, especially in the initial part of ones learning curve. A thorough knowledge of anatomy goes a long way in avoiding most of the complications seen in hernia repair. This anatomy needs to be relearned from what one is used to, as the approach is totally different from an open hernia repair. And finally, learning and mastering the right technique is an essential prerequisite before one ventures into inguinal hernia repair.”
“The most important preoperative precaution is proper patient selection prior to surgery, especially in the initial part of the learning curve. Ideally, direct or small indirect hernias are best. Large hernias, obese patients and irreducible, obstructed hernias are best avoided. An absolute contraindication is strangulated hernia. Also a detailed work-up of elderly patients to assess cardiorespiratory status is mandatory to ensure a safe outcome.”
Continue reading