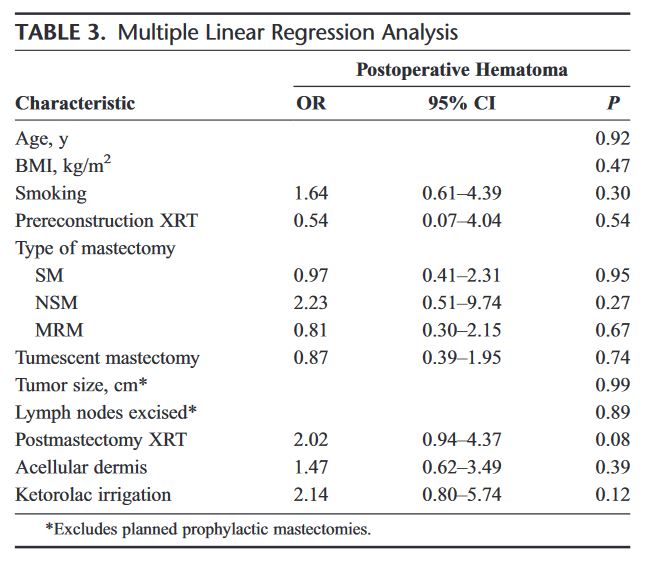
Case Presentation: “A 60-year-old male has been in the post-anesthetic care unit (PACU) for 6 hours with a slowly expanding neck hematoma following an uneventful left carotid endarterectomy under general anesthesia.”

Case Presentation: “A 60-year-old male has been in the post-anesthetic care unit (PACU) for 6 hours with a slowly expanding neck hematoma following an uneventful left carotid endarterectomy under general anesthesia.”
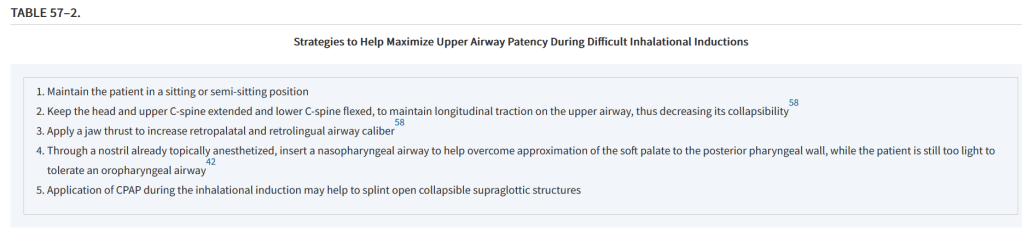
“Mesenteric bleeding (MB) occurs rarely and its frequency is not well known. It corresponds to bleeding from mesenteric vessels in the abdominal cavity, without intra-luminal digestive bleeding. Although relatively rare, this pathology can be life-threatening if left undiagnosed and untreated. Clinically, MB are characterized by non-systematised abdominal pain and sudden blood loss. MB has many causes such as a post operative complication (especially after pancreaticoduodenectomy), traumatism, tumour, or may be idiopathic with no cause found. CT-scan is the gold standard of diagnostic imaging to identify the cause of MB. While the management of upper and lower gastrointestinal bleeding has been well established, the management of active mesenteric bleeding is less defined in the medical literature.”
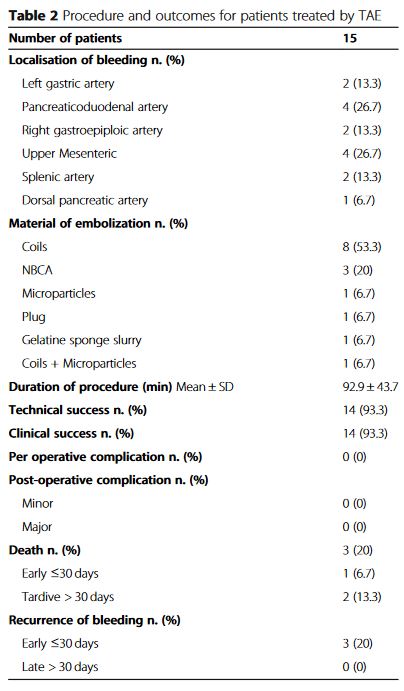
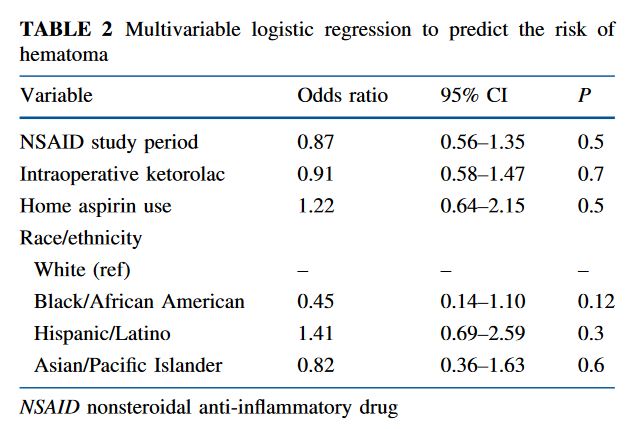
“Although the risk of postoperative bleeding is inherent to all surgical subspecialties, the development of a hematoma after mastectomy with implant reconstruction involves unique risk factors, including the routine involvement of 2 distinct surgical teams. However, despite numerous studies reporting their outcomes following these operations, a rigorous analysis of individual andcoperative factors that contribute to postoperative hematoma formation
has never been documented.”
“Among patients undergoing lumpectomy and Sentinel Lymph Node Biopsy with multimodal analgesia, the risk of hematoma in the 30-day postoperative period, including hematoma requiring reoperation and in-office aspiration or drainage, was low overall and not statistically significantly higher despite increased use of intraoperative ketorolac and implementtion of a standard discharge regimen of NSAIDs in lieu of opioids.”
Balzer KM, et al. Anatomic guidelines for the prevention of abdominal wall hematoma induced by trocar placement. Surg Radiol Anat. 1999;21(2):87-9. Full-text for Emory users.
Abstract: A knowledge of the parietal structures of the abdominal wall is necessary to minimize risks of operative procedures like laparoscopy. For means to prevent intraoperative bleeding and the occurrence of abdominal wall hematoma, we studied the course of the inferior epigastric arteries and the ascending branch of the deep circumflex iliac artery in 21 human cadavers. The abdominal wall structures were dissected and the distances of the arteries in relation to anatomic structures such as the umbilicus, pubic symphysis, superior ischial spine and lower edge of the rib-cage were measured. Comparison of the morphometric results obtained with the location of 36 trocar incision sites recommended in the common literature yields the information that about half of these incision sites incur the risk of injuring the arteries.
Continue reading