One discussion last week involved cardiac arrest in the setting of hernia repair. The reference below was highlighted in the chief resident’s presentation.
Reference: Rafiq A, Skylar E, Bella JN. Cardiac evaluation and monitoring of patients undergoing noncardiac surgery. Health Services Insight. 2017 Feb 20; 9: 1178632916686074. doi: 10.1177/1178632916686074.
Summary: Cardiovascular complications in the perioperative period are one of the most common events leading to increased morbidity and mortality. Although such events are very small in number, they are associated with a high mortality rate making it essential for physicians to understand the importance of perioperative cardiovascular risk assessment and evaluation. Its involves a detailed process of history taking, patient’s medical profile, medications being used, functional status of the patient, and knowledge about the surgical procedure and its inherent risks.
That being said, this review by Rafiq et al (2017) aims to provide a concise but comprehensive analysis on all such aspects of perioperative cardiovascular risk assessment for noncardiac surgeries and provide a basic methodology toward such assessment and decision making.
The ideal approach toward perioperative cardiac risk assessment requires a multidisciplinary team or a dedicated perioperative team of physicians. This leads expert physicians in this field to be involved in patient care with improved communications among primary physicians, anesthesiologist, surgeons, the patient, family members of the patient, cardiologist, and all other ancillary departments of health care involved.
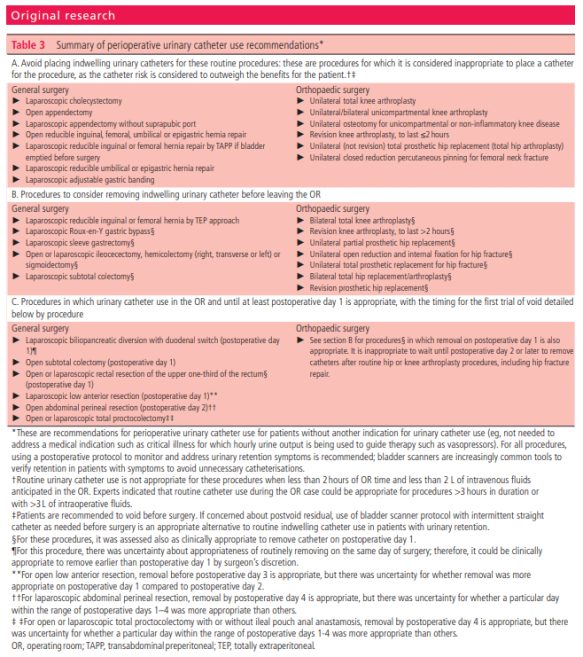
Figure 1: Algorithm for perioperative cardiac risk assessment prior to noncardiac surgery (p.2)

The authors state that it is important to stress the fact that a majority of these recommendations are based, to a large extent, on observational studies and clinical experience. There are only few RCTs that address this matter. It is prudent that more randomized trials are needed to improve on current recommendations, hence leading to further improvement in patient care and management in the perioperative period.