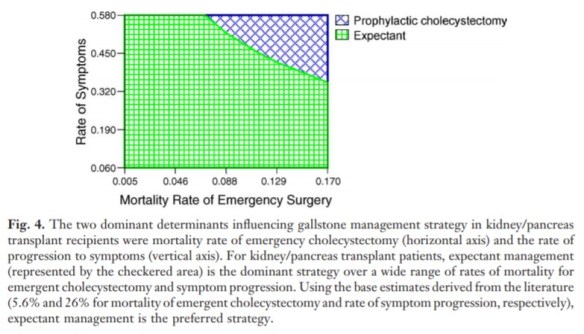
Kao LS, Flowers C, Flum DR. Prophylactic cholecystectomy in transplant patients: a decision analysis. J Gastrointest Surg. 2005 Sep-Oct;9(7):965-72.
Full-text for Emory users.
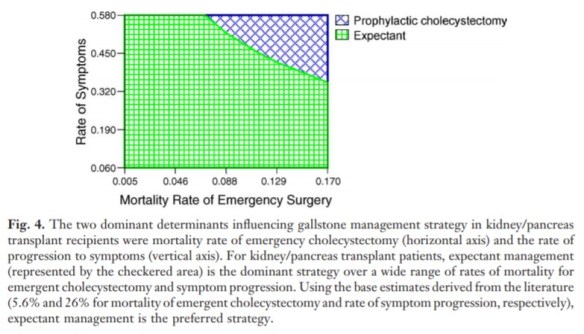

Kao LS, Flowers C, Flum DR. Prophylactic cholecystectomy in transplant patients: a decision analysis. J Gastrointest Surg. 2005 Sep-Oct;9(7):965-72.
Full-text for Emory users.
Dr. Steven M. Strasberg referenced the following citations during his presentation, “Understanding and Preventing Bile Duct Injury” on November 14, 2019.
Cho JY, Baron TH, Carr-Locke DL, et al. Proposed standards for reporting outcomes of treating biliary injuries. HPB (Oxford). 2018 Apr;20(4):370-378.
Strasberg SM. A three-step conceptual roadmap for avoiding bile duct injury in laparoscopic cholecystectomy: an invited perspective review. J Hepatobiliary Pancreat Sci. 2019 Apr;26(4):123-127.
Strasberg SM. Error traps and vasculo-biliary injury in laparoscopic and open cholecystectomy. J Hepatobiliary Pancreat Surg. 2008;15(3):284-92.
One discussion last week included classification of bile duct injuries.
Seeras K, Kalani AD. Bile Duct Repair. 2018 Nov 24. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.
Clinical Significance: “Many major bile duct injuries will require surgical repair. There are many described techniques for complex biliary injury repairs including primary repair or primary end to end anastomosis of bile ducts, choledochoduodenostomy, and cholecystojejunostomy. The most popular surgical repair is the Roux-en-Y hepaticojejunostomy. This operation has been consistently superior to the other methods when considering long-term outcomes. There are many different techniques described to perform an RYHJ, and the operating surgeon should choose the method with which he or she is most comfortable or experienced.”
A discussion in December compared early versus delayed cholecystectomy.
References: Ackerman J, et al. Beware of the interval cholecystectomy. The Journal of Trauma and Acute Care Surgery. 2017 Jul;83(10):55-60. Full-text for Emory users.
Gurusamy KS, Davidson C, Gludd C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis (Review). Cochrane Database of Systematic Reviews. 2013 Jun 30;(6):CD005440. Full-text for Emory users.
Summary: Cochrane’s review on early vs delayed cholecystectomy included 6 trials and 488 individuals. Of those, 244 received laparoscopic cholecystectomy early (within 7 days of presentation), while the remaining 244 received it at least 6 weeks after index admission with acute cholecystitis. The primary conclusion is that “based on information from a varied number of participants as well as trials at high risk of bias, early laparoscopic cholecystectomy during acute cholecystitis appears safe and shortens the total hospital stay [by 4 days]” (p.2).
There was no significant difference in operating time. Only one of the trials measured time to return to work, nothing that patients in the early group returned to work an average of 11 days earlier than the delayed group. Four trials did not report any gallstone-related complications; one trial reported five, including two people with cholangitis. In five trials, one-sixth of people in the delayed group had either non-resolution or recurrence of symptoms before their planned operation and had to have emergency laparoscopic cholecystectomy (p.6).
Using the terms immediate and interval, Ackerman et al (2017) conducted a retrospective cohort analysis to quantify the morbidity and mortality associated with a delayed, or interval cholecystectomy (IC). Of all patients admitted to 7 hospitals within the same healthcare system, 337 had percutaneous cholecystostomy (PC), 177 (52.5%) of those also had an interval cholecystectomy (IC). The table below illustrates the outcomes:

(Ackerman et al, 2017, p.57)