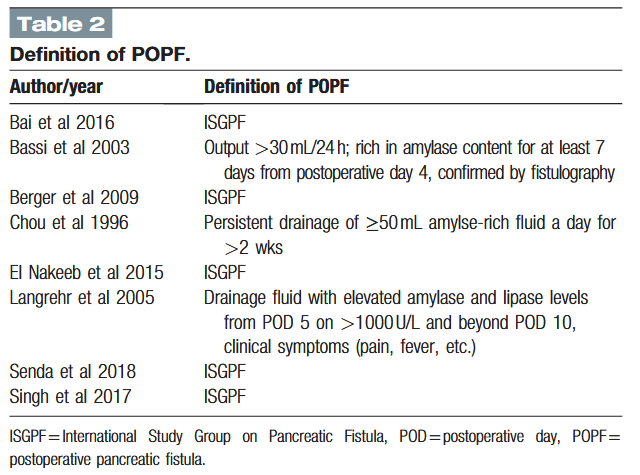
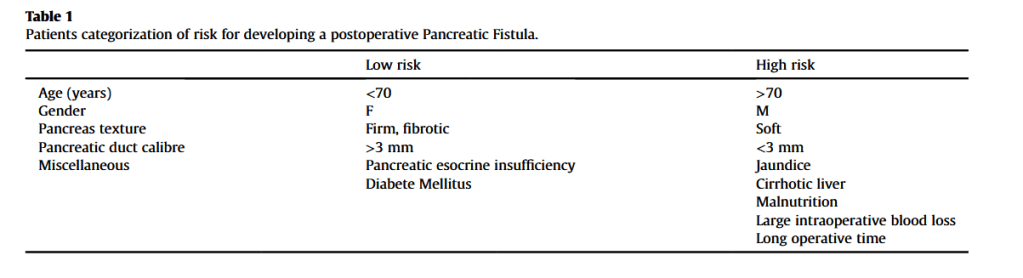
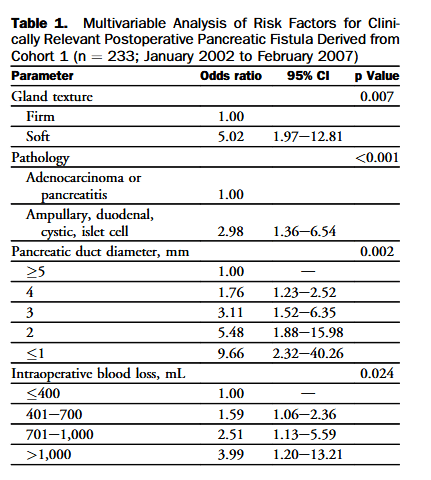
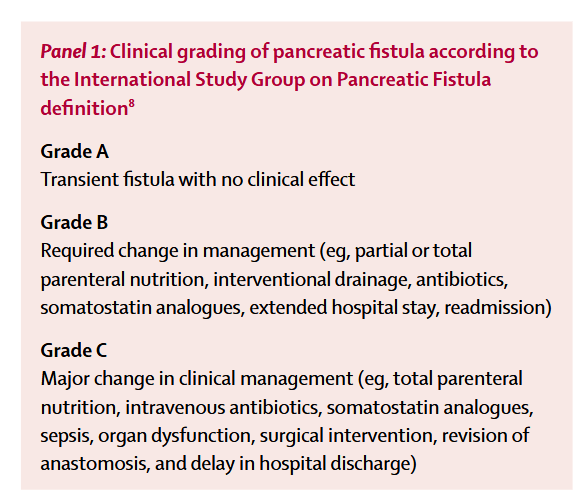
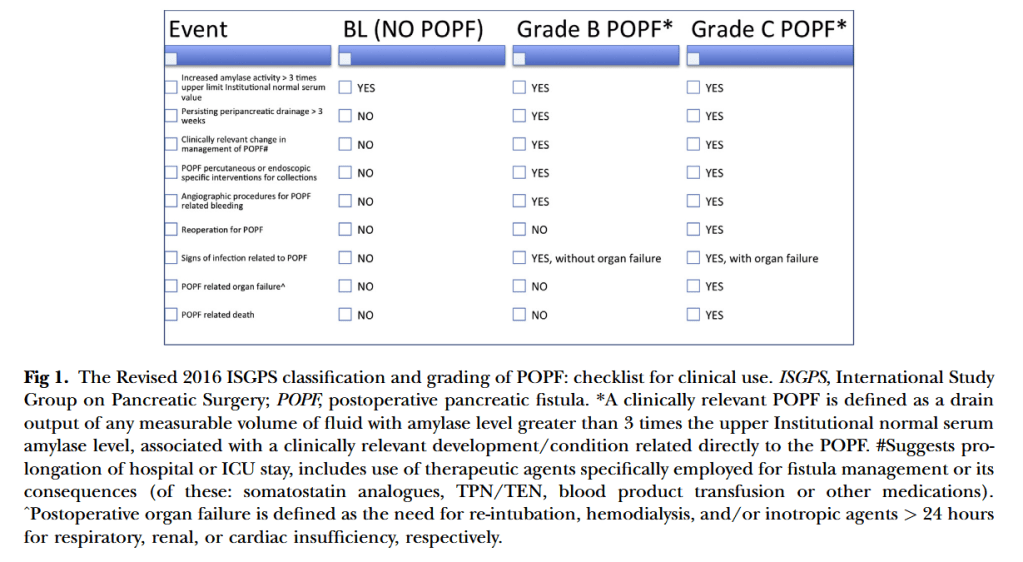
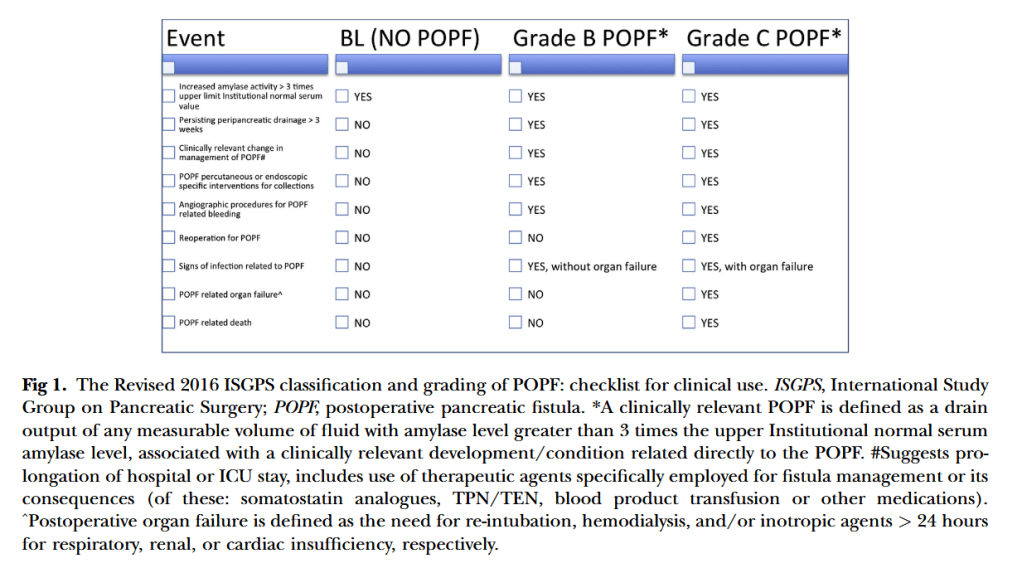
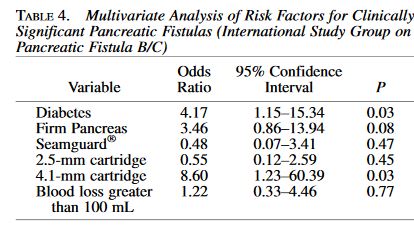
“Pancreaticoduodenectomy (PD) is a complex, high-risk standard surgical procedure that is indicated primarily for periampullary diseases. Central to the entire discipline of PD are postoperative mortality and morbidity. Although operative mortality in patients undergoing PD has decreased, the incidence of postoperative morbidity remains high at 40% to 50%. Postoperative pancreatic fistula (POPF) is the most common complication, with rates ranging from 5% to 30% in previous studies. Many methods have been described to decrease the risk of POPF, including the use of medications (prophylactic octreotide, sealants), prophylactic pancreatic stenting, and improvements in pancreatic reconstruction techniques. The most commonly used pancreatic reconstruction techniques are pancreaticogastrostomy (PG) and pancreaticojejunostomy (PJ).”