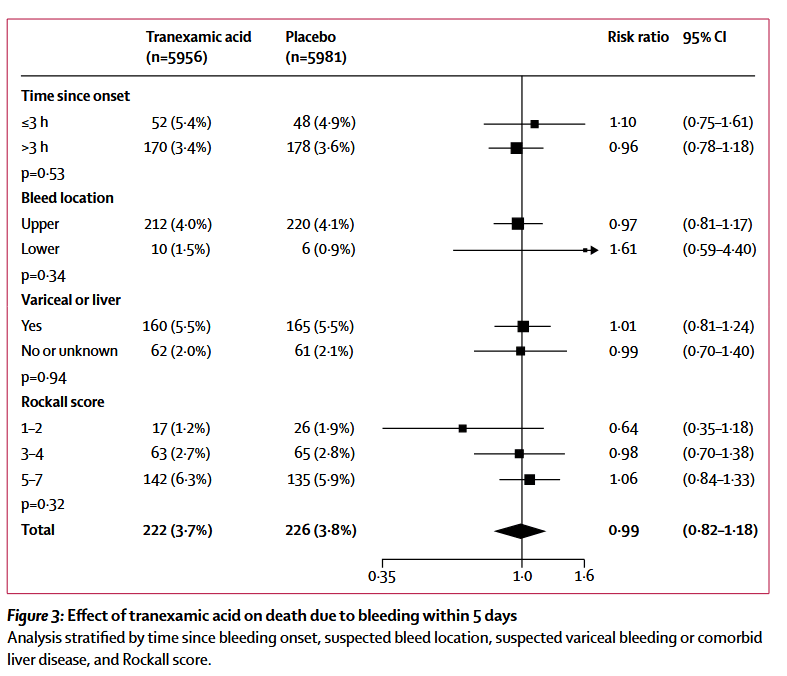
“Acute severe gastrointestinal bleeding is a common cause of death worldwide. Bleeding can occur from the upper or lower gastrointestinal tract, but upper gastrointestinal bleeding is more common. The leading causes are peptic ulcer, oesophageal varices, and malignancy. The case fatality rate is approximately 10% for upper gastrointestinal bleeding and 3% for lower gastrointestinal bleeding. Many patients re-bleed after initial haemostasis and those that do have a four times increased risk of death. Patients with acute severe gastrointestinal bleeding usually present with haematemesis or melaena. Patients are often haemodynamically unstable and in need of urgent resuscitation. Acute management
of gastrointestinal bleeding includes blood product transfusion, medical or endoscopic therapy, and surgery.”