“Top Take-Home Messages
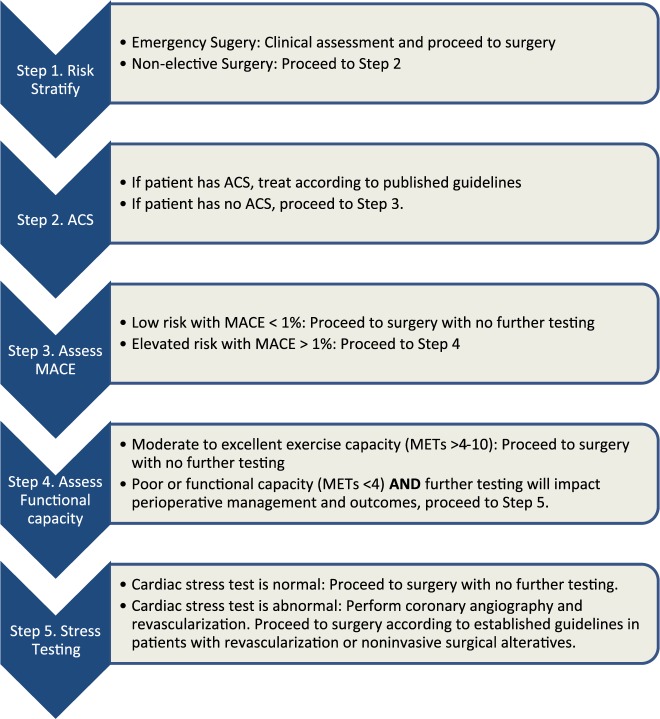
| 1. | A stepwise approach to perioperative cardiac assessment assists clinicians in determining when surgery should proceed or when a pause for further evaluation is warranted. | ||||
| 2. | Cardiovascular screening and treatment of patients undergoing noncardiac surgery should adhere to the same indications as nonsurgical patients, carefully timed to avoid delays in surgery and chosen in ways to avoid overscreening and overtreatment. | ||||
| 3. | Stress testing should be performed judiciously in patients undergoing noncardiac surgery, especially those at lower risk, and only in patients in whom testing would be appropriate independent of planned surgery. | ||||
| 4. | Team-based care should be emphasized when managing patients with complex anatomy or unstable cardiovascular disease. | ||||
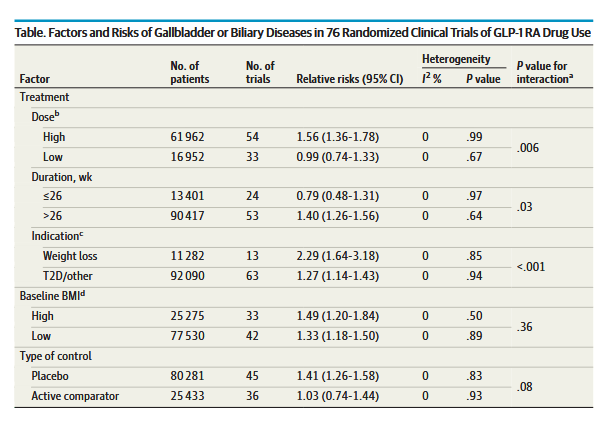
| 5. | New therapies for management of diabetes, heart failure, and obesity have significant perioperative implications. Sodium-glucose cotransporter 2 inhibitors should be discontinued 3 to 4 days before surgery to minimize the risk of perioperative ketoacidosis associated with their use. | ||||
| 6. | Myocardial injury after noncardiac surgery is a newly identified disease process that should not be ignored because it portends real consequences for affected patients. | ||||
| 7. | Patients with newly diagnosed atrial fibrillation identified during or after noncardiac surgery have an increased risk of stroke. These patients should be followed closely after surgery to treat reversible causes of arrhythmia and to assess the need for rhythm control and long-term anticoagulation. | ||||
| 8. | Perioperative bridging of oral anticoagulant therapy should be used selectively only in those patients at highest risk for thrombotic complications and is not recommended in the majority of cases. | ||||
| 9. | In patients with unexplained hemodynamic instability and when clinical expertise is available, emergency focused cardiac ultrasound can be used for perioperative evaluation; however, focused cardiac ultrasound should not replace comprehensive transthoracic echocardiography.” | ||||

∗Cardiovascular risk factors: hypertension, smoking, high cholesterol, diabetes, women age >65 y, men age >55 y, obesity, family history of premature CAD. †Determining elevated calculated risk depends on the calculator used. Traditionally, RCRI >1 or a calculated risk of MACE with any perioperative risk calculator >1% is used as a threshold to identify patients at elevated risk. §Abnormal biomarker thresholds: troponin >99th percentile URL for the assay; BNP >92 ng/L, NT-proBNP ≥300 ng/L. ‡Conditions that pose additional risk for MACE. ‖Noninvasive stress testing or CCTA suggestive of LM or multivessel CAD. Colors correspond to Class of Recommendation in Table 3. BNP indicates B-type natriuretic peptide; CABG, coronary artery bypass grafting; CAD, coronary artery disease; CCTA, coronary computed tomography angiography; CIED, cardiovascular implantable electronic device; CVD, cardiovascular disease; DASI, Duke Activity Status Index; ECG, electrocardiogram; GDMT, guideline-directed management and therapy; ICD, implantable cardioverter-defibrillator; LM, left main; MACE, major adverse cardiovascular event; METs, metabolic equivalents; NCS, noncardiac surgery; NT-proBNP, N-terminal pro b-type natriuretic peptide; RCRI, Revised Cardiac Risk Index; and URL, upper reference limit.