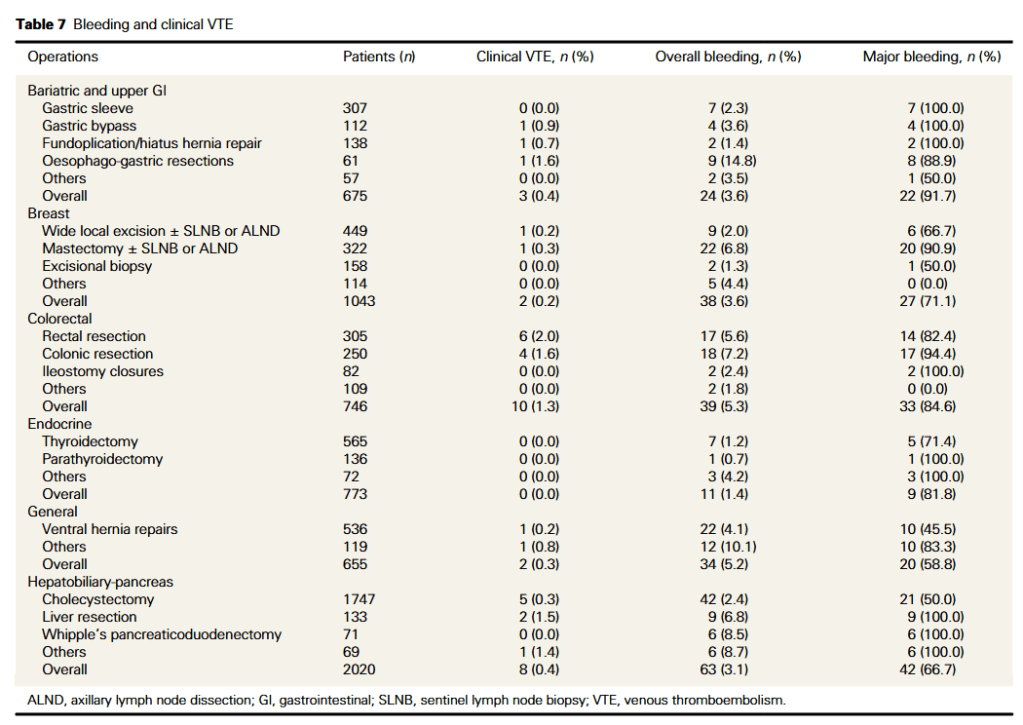
“General surgical patients who undergo major operations are at risk of venous thromboembolism (VTE). This incurs significant morbidity and healthcare costs. Therefore, the Royal Australasian College of Surgeons and other regulatory bodies recommend routine thromboprophylaxis. Moreover, considerations for thromboprophylaxis is an integral part of theatre timeout performed prior to any operation.”
“In this study, we extend the observations made from our multicentre survey by quantifying the heterogeneity of perioperative thromboprophylaxis across all major general surgical operations, and placing them in context of their bleeding and VTE risk. Findings from this study will highlight areas of practice with the greatest variability, allow surgeons to benchmark their practices against that of their colleagues and focus future research to optimize perioperative thromboprophylaxis.”