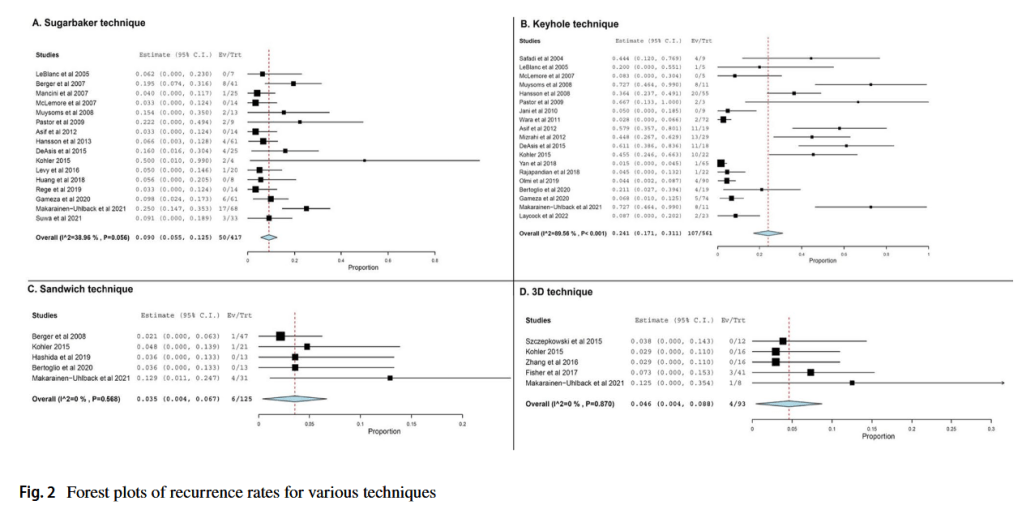
“The most commonly reported approaches for stomal hernia repair include stoma relocation, fascial repair using sutures, and fascial repair using prosthetic mesh with either open or minimally invasive surgery. At present, suture repair for elective surgery is no longer recommended due to high recurrence rates, except in specific circumstances such as
strangulation and contamination of the surgical field, where the use of mesh application should be avoided. In the last decade, many minimally invasive procedures have been
reported in the literature with varying results. In a previous systematic review in 2015, DeAsis et al. investigated the role of laparoscopic surgery in parastomal hernia repair and
concluded that the modified Sugarbaker technique demonstrated superior performance compared to other techniques. Likewise, the sandwich technique showed positive outcomes with low recurrence rates. In another study published in 2015, Szczepkowski et al. described an alternative approach called hybrid with three-dimensional (3D) meshes with promising results.