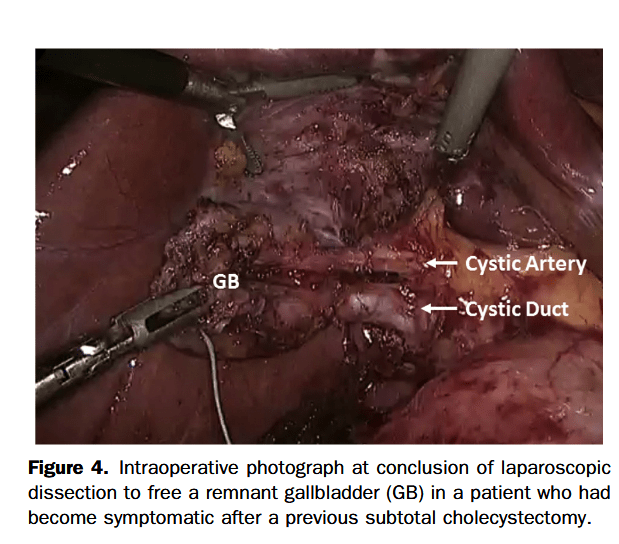
“Laparoscopic cholecystectomy is a well-established procedure with clear benefits for patients over open cholecystectomy. However, it is associated with an increased rate of
bile duct injury. Biliary injuries occur more commonly when operations are made more difficult due to the presence of severe acute and/or chronic inflammation. Under these conditions, secure ductal identification by the critical view of safety (CVS) may be very challenging because CVS requires clearing of the inflamed hepatocystic triangle in
order to demonstrate the cystic duct, cystic artery, and the cystic plate. It is a rigorous method, but as we have previously stressed, this is actually one of the strengths of the
CVS method of identification. The infundibular technique, in which the funnel-shaped infundibular-cystic duct junction is the rationale for identification, is much easier to achieve than CVS.”