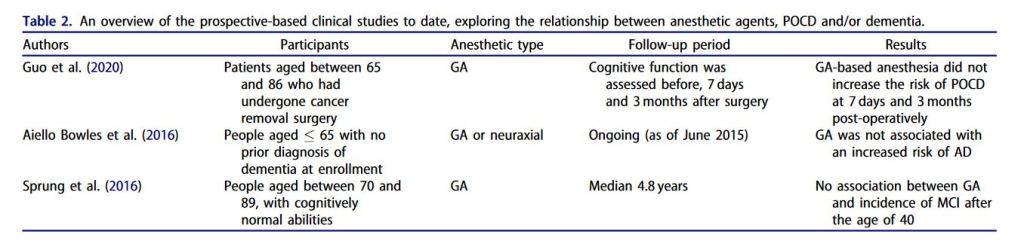
“Although the authors acknowledge that cognitive deterioration following surgery is a common phenomenon, there is little evidence that anesthesia itself or other surgical and patient factors can cause or accelerate cognitive decline and AD. The existing controversy in the field between animal and human studies highlights the need for transitioning from population-based studies to high-quality clinical studies especially with regards to dementia.” (Tsolaki)