“This study hypothesized that there may be additional differences between trauma surgery (TS) and emergency general surgery (EGS) patients, because the physiologic conditions are typically dominated by hemodynamic instability from hemorrhage in the former, whereas the latter is predominantly complicated by sepsis. The 2 groups may also have different patient demographics, with TS patients being younger and more likely to be male than EGS patients.”
Continue readingThe Landmark Series: Pancreatic Neuroendocrine Tumors
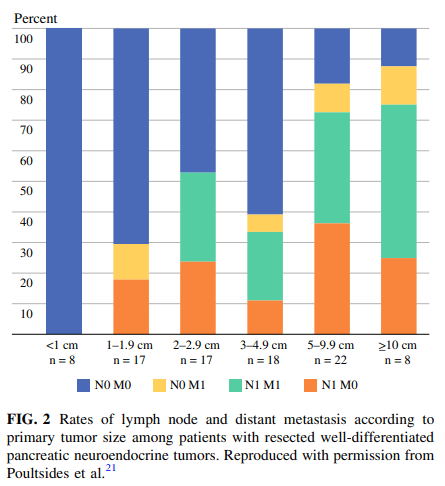
“Pancreatic neuroendocrine tumors (PNETs) comprise a heterogeneous group of neoplasms arising from pancreatic islet cells that remain relatively rare but are increasing in incidence worldwide. While significant advances have been made in recent years with regard to systemic therapies for patients with advanced disease, surgical resection remains the standard of care for most patients with localized tumors. Although formal pancreatectomy with regional lymphadenectomy is the standard approach for most PNETs, pancreas-preserving approaches without formal lymphadenectomy are acceptable for smaller tumors at low risk for lymph node metastases.”
Comparison of stapled versus handsewn loop ileostomy closure
“The purpose of this study was to compare the rates of small bowel obstruction, anastomotic complications, and wound infections between stapled and handsewn closures of loop ileostomies. The diverting loop ileostomy is a commonly used stoma, often employed to diminish the consequences of an anastomotic leak in low colorectal anastomoses, ileal pouch-anal anastomoses, and in situations where reversible patient factors increase the risk of an anastomotic dehiscence. They are also used to divert the fecal stream in the event of an anastomotic leak and, occasionally, in severe fistulizing perianal disease.”
Continue readingHandsewn vs. stapled anastomoses in colon and rectal surgery
“Trials comparing handsewn with stapled anastomoses in colon and rectal surgery have not found statistical differences. Despite this, authors have differed in their conclusions as to which technique is superior. To help determine whether differences in patient outcomes are present, a meta-analysis of all trials was performed.”
Continue readingMesh sutured repairs of the abdominal wall
“All high-tension internal surgical closures require that the ultimate tensile strength (UTS) of the repair remains greater than the forces applied. Otherwise, changes at the suture/tissue interface (STI) will lead to acute or chronic suture pull-through and surgical failure. For the abdominal wall, prophylactic flat meshes have been shown to improve outcomes of laparotomy closures and hernia repairs. Unfortunately, flat planar meshes have their own drawbacks, including increased time for placement, increased foreign material, increased tissue dissection, pain, infection, and cost.”
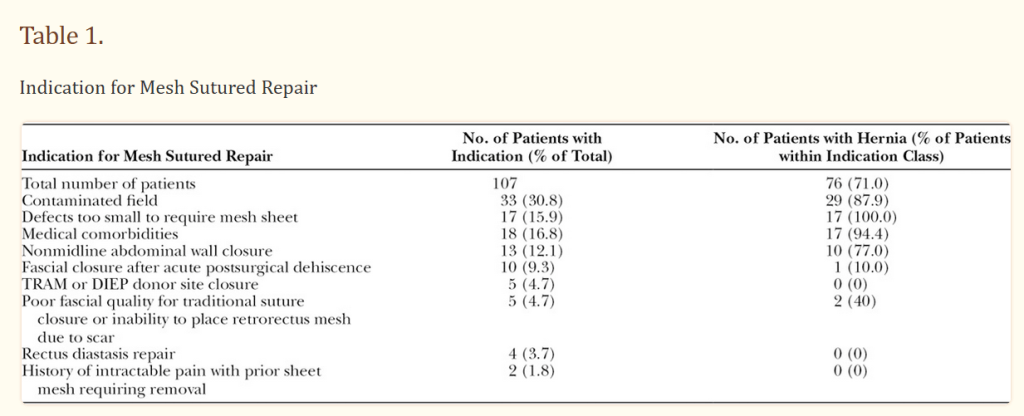
“One hundred and seven patients underwent a mesh sutured abdominal wall closure. Seventy-six patients had preoperative hernias, and the mean hernia width by CT scan for those with scans was 9.1 cm. Forty-nine surgical fields were clean-contaminated, contaminated, or dirty. Five patients had infections within the first 30 days. Only one knot was removed as an office procedure. Mean follow-up at 234 days revealed 4 recurrent hernias.”
Lanier, S. T., et al (2016). Mesh Sutured Repairs of Abdominal Wall Defects. Plastic and reconstructive surgery. Global open, 4(9), e1060. Free Full Text
Evaluation of the utility of placing an intra-abdominal drain in laparoscopic appendectomy for complicated acute appendicitis.
“Complicated appendicitis (CA) may be a risk factor for postoperative intra-abdominal
abscess formation (IAA). In addition, several publications have shown an increased risk of postoperative collection after laparoscopic appendectomy. Most surgeons prefer to place a drain to collect contaminated abdominal fluid to prevent consequent abscess formation. We aimed to evaluate the utility of placing an intra-abdominal drain in laparoscopic appendectomy for complicated acute appendicitis.”
“This study concludes the use of intra-abdominal drain in laparoscopic appendectomy for complicated acute appendicitis does not prevent postoperative complications and may even lengthen hospital stay. Larger and prospective studies are needed to achieve more definitive conclusions.”
Schlottmann F, et al Could an abdominal drainage be avoided in complicated acute appendicitis? Lessons learned after 1300 laparoscopic appendectomies. Int J Surg. 2016 Dec;36(Pt A):40-43 Free Full Text
Intraoperative cholangiography during laparoscopiccholecystectomy:
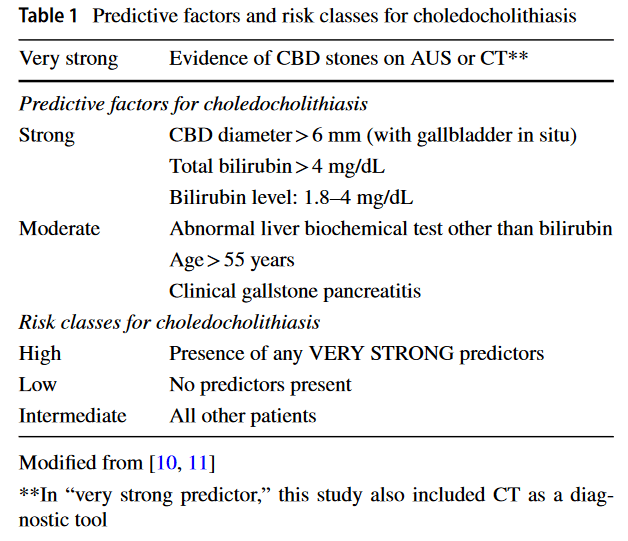
“Based on the study results, the 2016 WSES risk classes for choledocholithiasis could be an effective approach for predicting the risk of choledocholithiasis. Considering its advantages for detecting CBD stones and biliary injuries, the routine use of IOC is still suggested.” (Lai)