A multivariate analysis showed the following adverse risk factors for AL: age > 65 years, hemoglobin < 8.0 g/dL and malnourishment. A multivariable model for AL showed a strong optimism-adjusted discrimination (concordance index, 0.675).


A multivariate analysis showed the following adverse risk factors for AL: age > 65 years, hemoglobin < 8.0 g/dL and malnourishment. A multivariable model for AL showed a strong optimism-adjusted discrimination (concordance index, 0.675).

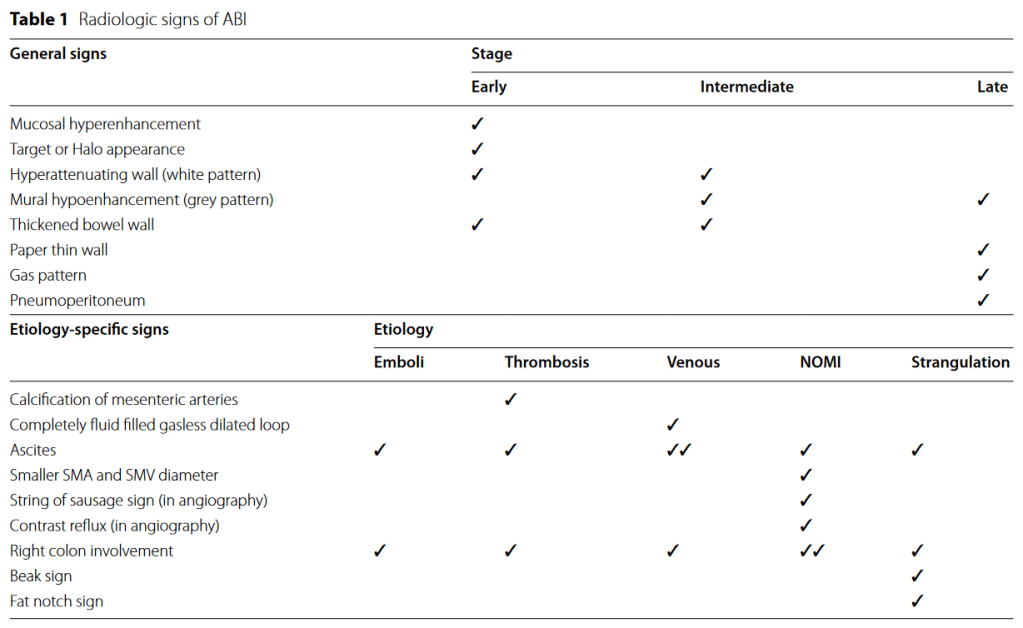
“Acute bowel ischemia (ABI) can be life threatening with high mortality rate. The radiologist plays a central role in the initial diagnosis and preventing progression to irreversible intestinal ischemic injury or bowel necrosis. The most single imaging findings described in the literature are either non-specific or only present in the late stages of ABI, urging the use of a constellation of features to reach a more confident diagnosis”
“The anatomical position of the inferior epigastric artery (IEA) subjects it to risk of injury during abdominal procedures that are close to the artery, such as laparoscopic trocar insertion, insertion of intra-abdominal drains, Tenckhoffâ catheter (peritoneal dialysis catheter) and paracentesis. This article aims to raise the awareness of the anatomical variations of the course of the IEA in relation to abdominal landmarks in order to define a safer zone for laparoscopic ancillary trocar placement. Methods of managing the IEA injury as well as techniques to minimise the risk of injury to the IEA are reviewed and discussed.”
Continue reading“The use of prophylactic ureteral stents remains controversial and could help in the intraoperative identification of ureteral injury.”
Methods:
Patients undergoing elective abdominal colorectal surgery and preoperative ureteral stent placement at three enterprise-wide tertiary referral hospitals between 2015 and 2021 were retrospectively identified through their billing records. The main study endpoint was ureteral injury identified within 30 days postoperatively. The decision to place ureteral stents was at the discretion of the treating surgeon. A number of demographic, disease-related, and treatment-related variables were examined for possible association with ureteral stent placement. We compared the incidence of ureteral injury and timing of the identification according to use of ureteral stents. Bivariate associations were examined using Kruskal-Wallis tests for continuous variables and Chi-square tests for categorical variables.
“Between January 1995 and April 2003, 1595 patients underwent PD for periampullary disease (392 benign, 1203 malignant). A retrospective analysis of a prospectively collected database was performed to determine the incidence of biliary stricture after PD.”
Results: “Forty-two of the 1595 patients (2.6%) who underwent PD developed postoperative jaundice secondary to a stricture of the biliary-enteric anastomosis. There was no difference in the incidence of biliary strictures after resection for benign (n = 10, 2.6%) or malignant disease (n = 32, 2.6%). The median time to stricture formation resulting in jaundice was 13 months (range, 1–106 months) and was similar for patients with benign and malignant disease. Preoperative jaundice did not protect against biliary stricture formation. By univariate analysis, biliary strictures were associated with preoperative percutaneous biliary drainage (odds ratio [OR] = 2.11, P = 0.02) and postoperative biliary stenting (OR = 2.11, P = 0.013). Postoperative chemoradiotherapy in patients with malignant disease was not associated with stricture formation. All strictures were initially managed with percutaneous biliary balloon dilatation and stenting, and only 2 patients required redo hepaticojejunostomy. Recurrent neoplastic disease was discovered in only 3 of the 32 patients (9%) with malignant disease. All 3 of these patients had cholangiocarcinoma as their initial diagnosis.”
Continue readingFerrara M, Kann BR. Urological injuries during colorectal surgery. Clin Colon Rectal Surg. 2019 May;32(3):196-203.
“A recent retrospective population-based study of patients in the United States undergoing colorectal surgery found the overall incidence of ureteral injury to be 0.28%. The incidence was found to be significantly higher in patients with stage 3 or 4 cancer, malnutrition, steroid use, and in operations done at teaching hospitals. Rectal cancer cases were found to have the highest rates of ureteral injuries (7.1/1,000), followed by Crohn’s disease and diverticular disease (2.9/1,000 each). In this review, laparoscopic surgery was associated with a lower incidence of ureteral injuries when compared with open (1.1 vs. 2.8/1,000, p < 0.001). Of the specific operations reviewed, abdominoperineal resection (APR) was found to have the highest rate of ureteral injury at 7.1/1,000 cases.” (Ferrara, 2019, p. 196)
Continue reading
We are excited to share a new section titled “Essential Articles for Surgical Residents.”
Keeping up with surgical literature in residency can be challenging. This list was created to serve as an easily accessible, up-to-date, and evidence-based resource for residents.
The content has been curated by faculty from each department and is intended to supplement the standard educational curriculum of each rotation with current and relevant literature.
Continue reading