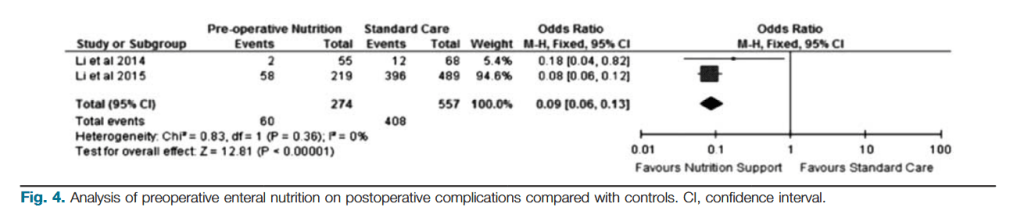
“Surgery is frequently needed in Crohn’s Disease (CD) patients who have malnutrition. Patients with CD are at a risk of malnutrition secondary to decreased oral intake, malabsorption, and inflammation. The prevalence of malnutrition in IBD patients is profound: 60–80% of IBD patients are anemic, 39–81% are iron deficient, 20–60% are vitamin B12
deficient, 36–54% are folate deficient, and 25–80% have hypoalbuminemia. This high prevalence of malnutrition presents a challenge in the surgical management of CD patients because poor preoperative nutritional status has been linked to increase postoperative complications.
Therefore, nutritional optimization using enteral nutrition (EN) and total parenteral nutrition (TPN) have been used for many years to improve the nutritional status of CD patients in hopes of decreasing postoperative complications.”