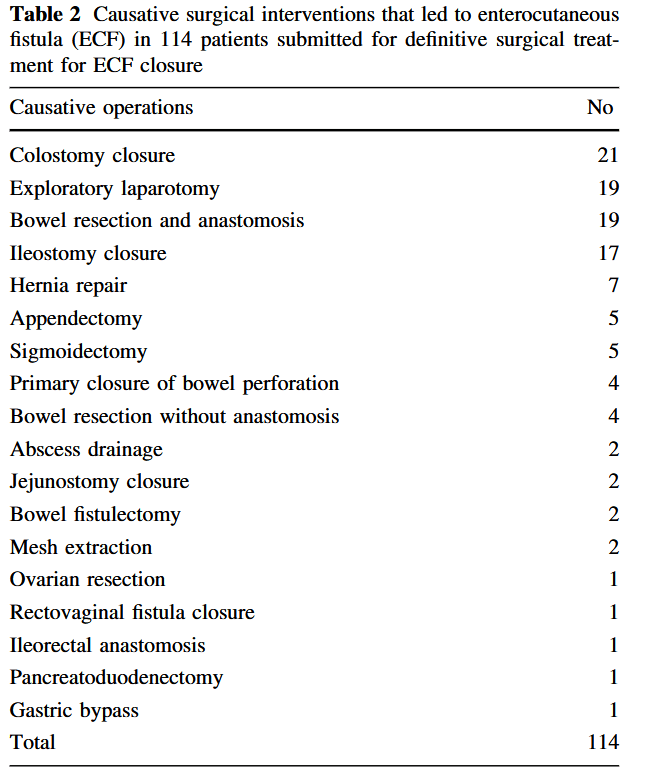
“In the case of enterocutaneous fistula (ECF) initial medical therapy aims to stabilize the patient, optimize the nutritional status and control of infections and fistula output. When surgery is required, extensive adhesiolysis, bowel resection and anastomosis along with abdominal wall reconstruction are necessary. The primary endpoint in patients undergoing surgical treatment with ECF as well as in the case of intestinal stomas, is to solve the intestinal defect, thus leaving in secondary terms other problems such as ventral hernias.
The simultaneous treatment of fistula/stoma closure with abdominal wall defect closure has been widely debated since some argue that the risk of complications such as anastomotic leakage is increased due to prolonged surgery and anesthetic time. However, various studies are reporting good results in patients undergoing simultaneous stoma with giant wall defect correction surgery, without increased risks and rates of complications.”