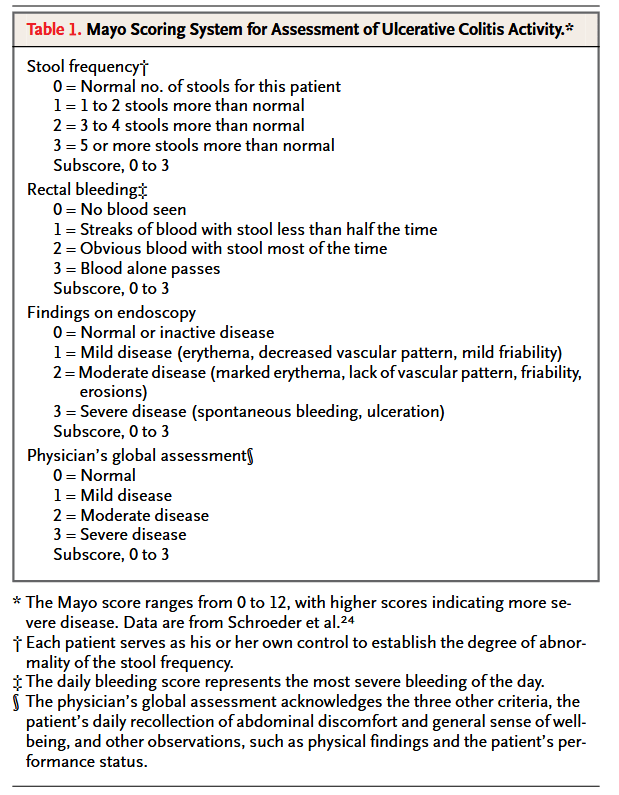
Ulcerative colitis is characterized by mucosal ulceration, rectal bleeding, diarrhea, and abdominal pain. Pharmacologic management of ulcerative colitis has relied mainly on 5-aminosalicylates, corticosteroids, and immunosuppressants, including purine antimetabolites and cyclosporine. Corticosteroid dependence is a clinically important problem; furthermore, the probability of colectomy within the first five years after diagnosis ranges from 9 percent in patients with distal colitis to 35 percent in patients with total colitis, most commonly because of failed medical therapy. The cumulative risk of recurrent inflammatory bowel disease in the form of pouchitis ranges from 15.5 percent one year after the procedure to 45.5 percent 10 years after the procedure. Accordingly, new treatments for ulcerative colitis are needed.”