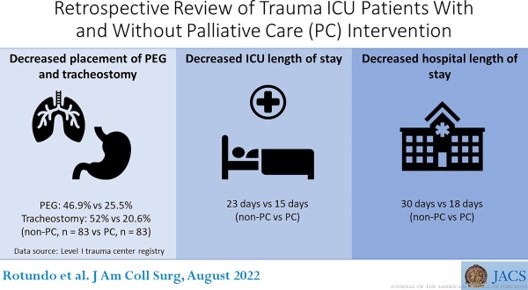
“Palliative care (PC) interventions in the critically ill have been associated with reduced subsequent ICU admissions and reduced ICU length of stay. Barriers to PC integration
and utilization in the ICU include unrealistic expectations of ICU interventions by patients and families, barriers related to ICU culture as well as cultural attributes of patients and families, insufficient training in PC principles for ICU clinicians, PC workforce shortages,
and inability of patients to participate in treatment discussions. Overcoming these barriers and assessing patient and provider needs for specialty PC depends on the availability and capabilities of PC services at the institutional level, the bandwidth of providers and characteristics of the patient population.”