Gad EH, et al. Laparoscopic cholecystectomy in patients with liver cirrhosis: 8 years experience in a tertiary center. A retrospective cohort study. Ann Med Surg (Lond). 2020 Jan 15;51:1-10. Free full-text.
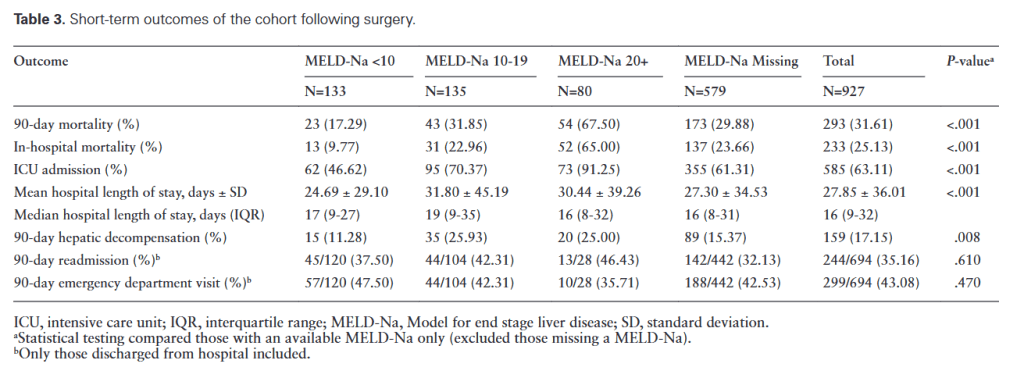
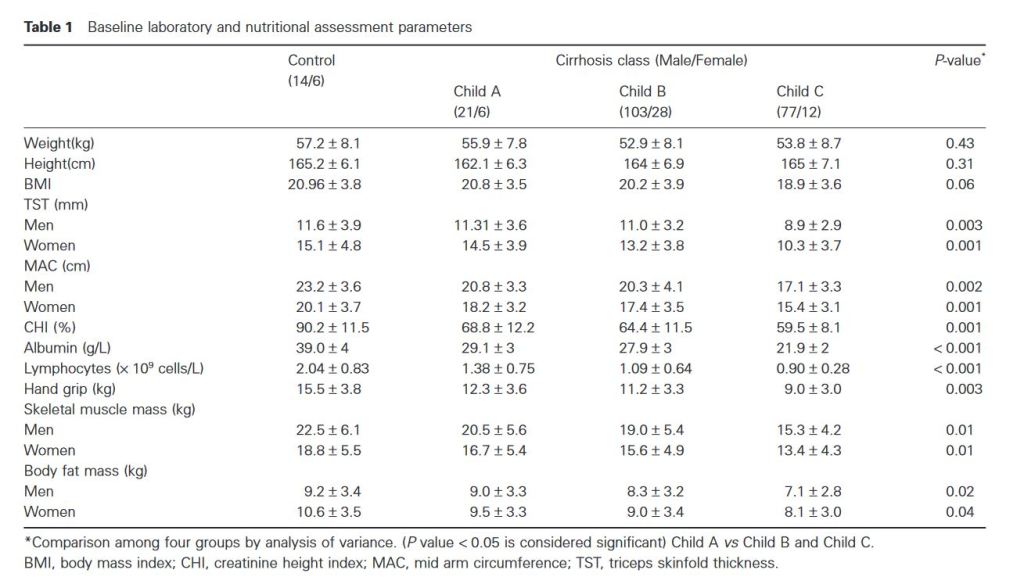
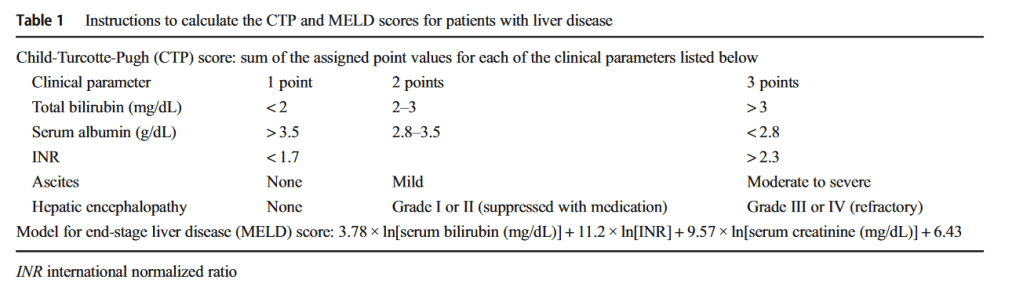
Results: The most frequent Child-Turcotte-Pugh (CTP) score was A, The most frequent cause of cirrhosis was hepatitis C virus (HCV), while biliary colic was the most frequent presentation. The harmonic device was used in 39.9% of patients, with a significant correlation between it and lower operative bleeding, lower blood and plasma transfusion rates, higher operative adhesions rates, lower conversion to open surgery and 30-day complication rates, shorter operative time and post-operative hospital stays where operative adhesions and times were independently correlated. The 30-day morbidity and mortality were 22.1% and 2.3% respectively while overall survival was 91.5%, higher CTP, and model for end-stage liver disease (MELD) scores, higher mean international normalization ratio (INR) value, lower mean platelet count, higher operative bleeding, higher blood, and plasma transfusion rates, longer mean operative time and postoperative hospital stays were significantly correlated with all conversion to open surgery, 30-day morbidities and mortalities.
Conclusion: LC can be safely performed in cirrhotic patients. However, higher CTP and MELD scores, operative bleeding, more blood and plasma transfusion units, longer operative time, lower platelet count, and higher INR values are predictors of poor outcome that can be improved by proper patient selection and meticulous peri-operative care and by using Harmonic scalpel shears.
Continue reading →