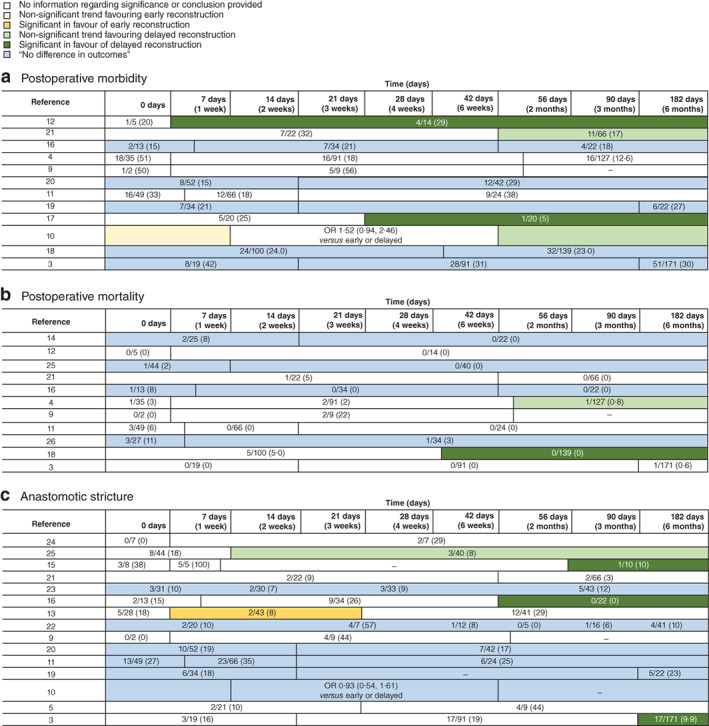
“One factor that may influence both short- and long-term outcomes of surgical reconstruction is the timing of surgical reconstruction. Delaying surgical reconstruction allows for optimization of the clinical condition of the patient as adequate sepsis control is achieved. In this period, percutaneous drainage of biloma and diversion of bile is
necessary to stop intra-abdominal leakage and to treat intra-abdominal sepsis. Immediate or early reconstruction, however, may reduce the burden for the patient and may prevent a decline in the clinical condition in the first place. Early reconstruction may also lead to shorter duration of hospital stay and thus reduce costs5 . Bile duct ischaemia, however, may still be developing at the time of an early repair, eventually causing strictures proximal to the level of the anastomosis. This is especially the case when there is concomitant vascular injury.”