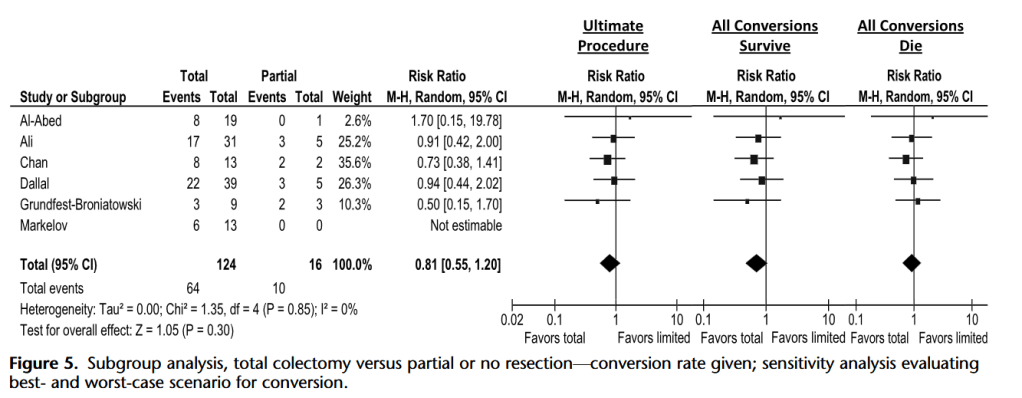
“Findings in the literature suggest that prompt surgical treatment of patients with fulminant Clostridium difficile-associated disease (CDAD) is necessary to ensure patient survival. However, controversy remains regarding the best surgical approach and timing. Recent efforts have been made in the creation of a scoring system to predict deterioration and improve patient care. New surgical approaches such as ileostomy and washout have shown promising results, but more rigorous data and longer follow-up, especially with regard to
disease recurrence after ileostomy reversal, are needed to evaluate the true value of these techniques regarding mortality.”