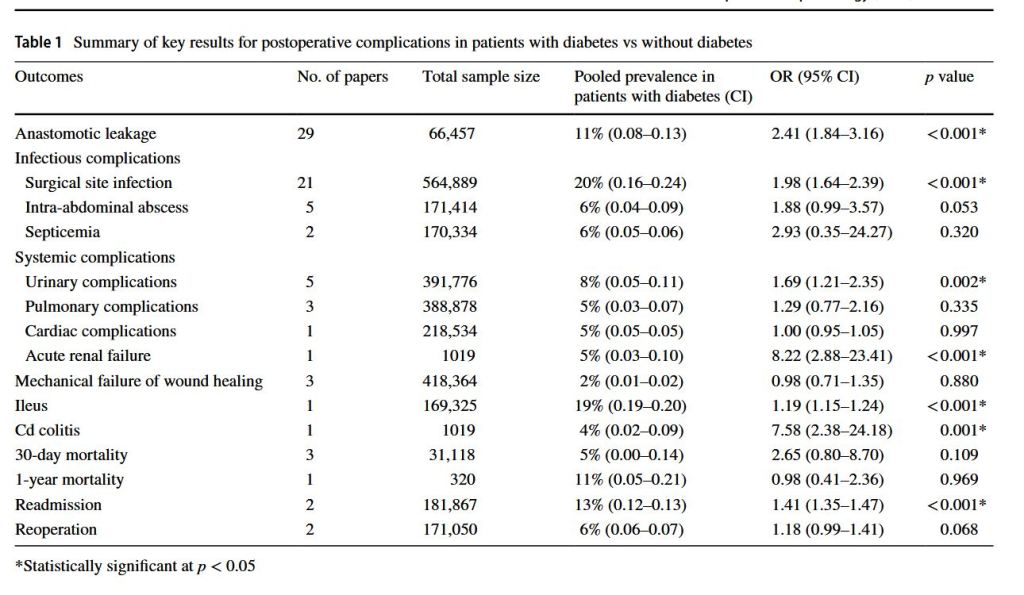
“Diabetes continues to be a significant comorbidity that needs to be accounted for during surgical planning. Furthermore, undiagnosed diabetes or ‘pre-diabetes’ results in an underestimation of the true number of patients with diabetes having colorectal
surgery, with studies reporting that the true prevalence of diabetes in hospitalised patients has been understated by up to 40%. In the existing literature, poor glycemic control and hyperglycemia has been associated with impaired wound healing and increased susceptibility to infections,leading to an elevated risk of postoperative complications.”