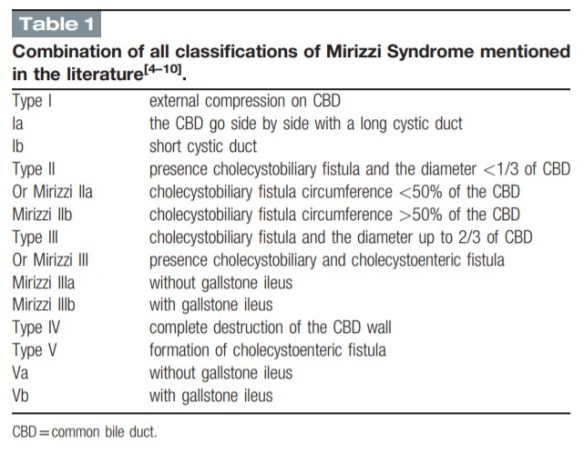
Chen H, Siwo EA, Khu M, Tian Y. Current trends in the management of Mirizzi Syndrome: A review of literature. Medicine (Baltimore). 2018 Jan;97(4):e9691.
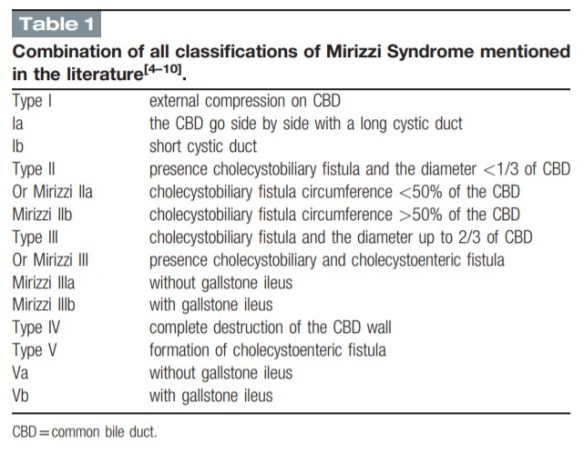

Chen H, Siwo EA, Khu M, Tian Y. Current trends in the management of Mirizzi Syndrome: A review of literature. Medicine (Baltimore). 2018 Jan;97(4):e9691.
Pomposelli Frank, and Gilbert Upchurch. Fischer’s Mastery of Surgery, edited by Josef E. Fischer, et al., Wolters Kluwer, 2011. ProQuest Ebook Central.
Continue readingEmory users, open this instance of PubMed, then click the links below for full-text article access.
Khan JM, et al. Transcatheter Electrosurgery: JACC State-of-the-Art Review J Am Coll Cardiol. 2020 Mar 31;75(12):1455-1470. doi: 10.1016/j.jacc.2020.01.035.
Editors. American Association for Thoracic Surgery/International Society for Heart and Lung Transplantation guidelines on selected topics in mechanical circulatory support J Heart Lung Transplant. 2020 Mar;39(3):187-219. doi: 10.1016/j.healun.2020.01.1329.
Giustino G, et al. Mortality After Repeat Revascularization Following PCI or CABG for Left Main Disease: The EXCEL Trial JACC Cardiovasc Interv. 2020 Feb 10;13(3):375-387. doi: 10.1016/j.jcin.2019.09.019.
Holm NR, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: updated 5-year outcomes from the randomised non-inferiority NOBLE trial Lancet. 2020 Jan 18;395(10219):191-199. doi: 10.1016/S0140-6736(19)32972-1.
Seese L, et al. The Impact of Major Postoperative Complications on Long-Term Survival After Cardiac Surgery Ann Thorac Surg. 2020 Jul;110(1):128-135. doi: 10.1016/j.athoracsur.2019.09.100.
Continue readingChampagne BJ, et al. Outcome of aggressive surveillance colonoscopy in ruptured abdominal aortic aneurysm. J Vasc Surg. 2004 Apr;39(4):792-6.
Purpose: Emergent repair of ruptured abdominal aortic aneurysms (rAAAs) is associated with high perioperative morbidity and mortality. One of the significant complications of this surgery is bowel ischemia. Reports detail mortality as high as 80% when this condition is realized. The objective of this project was to determine both the incidence and the effect of mandatory postoperative colonoscopy on outcome of colon ischemia after rAAA.
Methods: From July 1995 to September 2002 all patients with an rAAA who underwent emergent aortic reconstruction were included in this review. All colonoscopies were performed within 48 hours, ischemia was graded consistently, and treatment was initiated per protocol based on grade of ischemia. Patients with grades I and II ischemia were followed up with medical management and repeat colonoscopy. All patients with grade III ischemia underwent bowel resection. Preoperative, intraoperative, and postoperative variables were collected to assess possible independent risk factors for and predictors of bowel ischemia.
Continue reading| Emory users, open this instance of PubMed, then click the links below for full-text article access. |
McMasters KM. Introducing: The Landmark Series. Ann Surg Oncol. 2020 Jan;27(1):1-2.
The Annals of Surgical Oncology, the journal of the Society of Surgical Oncology, has created The Landmark Article Series.
“The Landmark Series is designed to trace the origins of current multidisciplinary therapy for each type of solid tumor, and demonstrate the logical progression of clinical trials and other key evidence. It is meant to be an educational resource, for trainees and practicing cancer specialists alike, in the understanding of evidence-based cancer management. Practice-changing clinical trials and other key evidence that inform our current treatment guidelines will be summarized and reviewed. Expert authors will provide context and commentary to enhance the value to the reader.” (McMasters, p.1).
See the most current collection of articles sorted by disease site here. Emory users, use this link to access the full-text.
Beasley GM, et al. The Landmark Series: Regional Therapy of Recurrent Cutaneous Melanoma. Ann Surg Oncol. 2020 Jan;27(1):35-42.
Egger ME, et al. The Sunbelt Melanoma Trial. Ann Surg Oncol. 2020 Jan;27(1):28-34.
Bello DM, Faries MB. The Landmark Series: MSLT-1, MSLT-2 and DeCOG
(Management of Lymph Nodes). Ann Surg Oncol. 2020 Jan;27(1):15-21.
Jolissaint JS, et al. Timing and Outcomes of Abdominal Surgery in Neutropenic Patients. J Gastrointest Surg. 2019 Apr;23(4):643-650.
Full-text for Emory users.
Results: Amongst 237 patients, mortality was 11.8% (28/237) and morbidity 54.5% (130/237). Absolute neutrophil count < 500 cells/μL (50% vs. 20.6%, P < 0.01) and perforated viscus (35.7% vs. 14.8%, P = 0.01) were associated with mortality. Perforated viscus (25.4% vs. 7.5%) was also associated with morbidity. Urgent operations were associated with higher morbidity (63.6% vs 34.7%, P < 0.001) and mortality (16.4% vs 1.4%, P = 0.002) when compared to elective operations. Transfer from an outside hospital (22.3% vs. 11.2%, P = 0.02) and longer median time from admission to operation (2 days (IQR 0-6) vs. 1 day (IQR 0-3), P < 0.01) were associated with morbidity. An ANC threshold of 350 provided the best discrimination for mortality.
Conclusions: Elective surgery in the appropriately chosen neutropenic patient is relatively safe. For patients with obvious surgical pathology, we advocate for earlier operation and a lower threshold for surgical consultation in an effort expedite the diagnosis and necessary treatment.
Continue readingDi Saverio S, et al. Pancreas-sparing, ampulla-preserving duodenectomy for major duodenal (D1-D2) perforations. Br J Surg. 2018 Oct;105(11):1487-1492.
Results: Ten patients were treated with this technique; seven had perforated or bleeding peptic ulcers, two had iatrogenic perforations and one blunt abdominal trauma. Their mean age was 78 (range 65-84) years. Four patients were haemodynamically unstable. The location of the duodenal injury was always D1 and/or D2, above or in close proximity to the ampulla of Vater. The surgical approach was open in nine patients and laparoscopic in one. The mean duration of surgery was 264 (range 170-377) min. All patients were transferred to the ICU after surgery (mean ICU stay 4·4 (range 1-11) days), and the overall mean hospital stay was 17·8 (range 10-32) days. Six patients developed major postoperative complications: cardiorespiratory failure in five and gastrointestinal complications in four. Surgical reoperation was needed in one patient for postoperative necrotizing and bleeding pancreatitis. Two patients died from their complications.
Continue reading