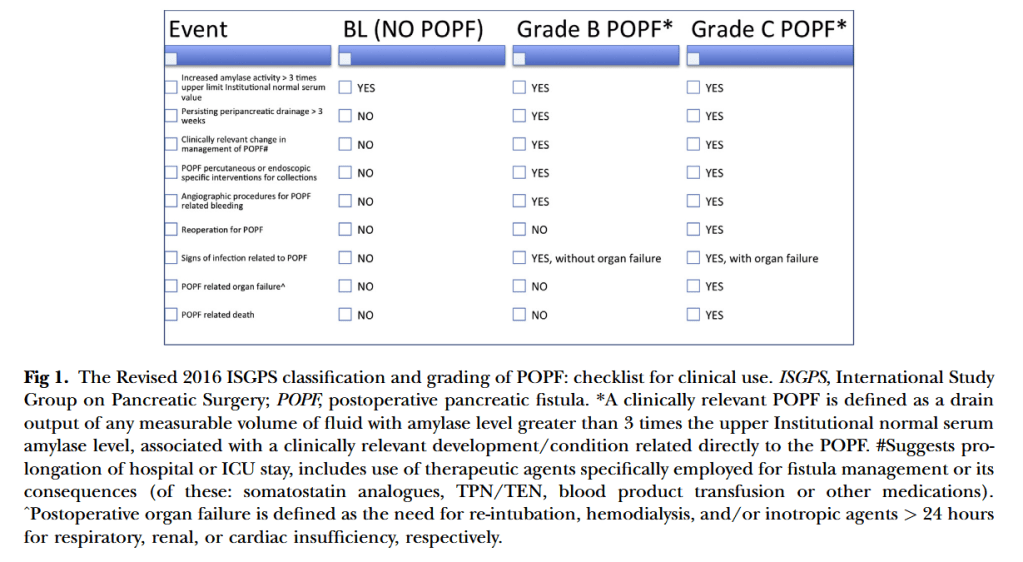
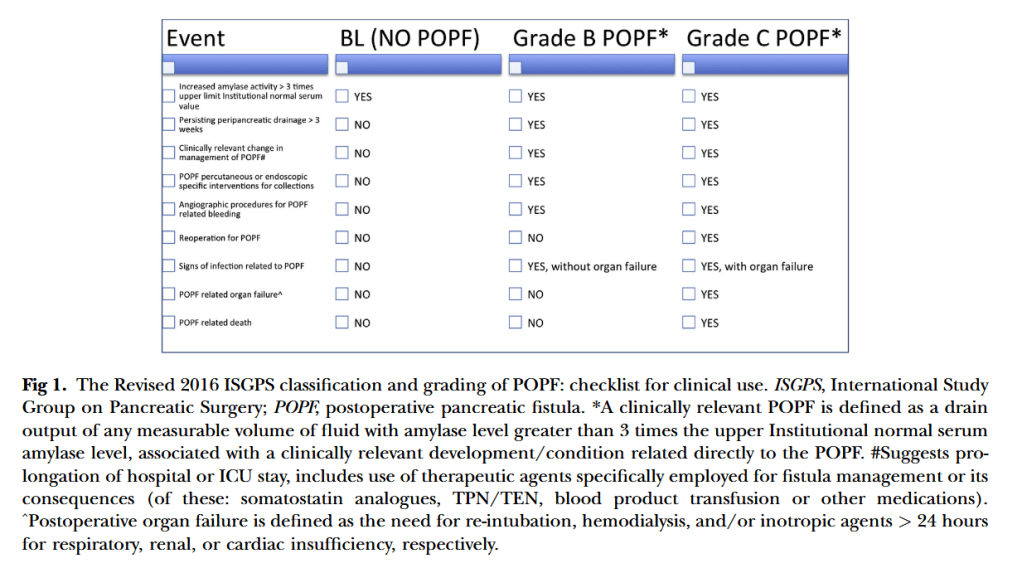
“Eleven years after its definition, postoperative pancreatic fistula (POPF) still remains one of the most harmful complications after pancreatic resection. Despite all the advances and technical modifications developed during this past decade to prevent POPF, the incidence of this dreaded complication still ranges between 3–45 % of pancreatic operations at high-
volume centers. Updating the ISGPF classification is both relevant and clinically important,
because POPF remains the single main determinant of serious postoperative morbidity and mortality related to pancreatic resection and plays a major role in terms of operation-related mortality, morbidity, hospital stay, and economic impact.”